The lower limb is the most common site for wounds (Guest et al, 2015) and, with almost half being considered ‘chronic’ or complex (Guest et al, 2017), it is essential that timely, appropriate treatment is provided to increase the chances of healing, improve patient quality of life and reduce pressure on healthcare services. There is currently a lack of wound differentiation, marked variation in care and underuse of evidence-based interventions in practice (Guest et al, 2015; Gray et al, 2018). Making a clear diagnosis and integrating wound care into the management of underlying comorbidities will address these issues. As patients are often treated across several healthcare settings, success will depend on multidisciplinary care in conjunction with clear treatment and referral pathways.
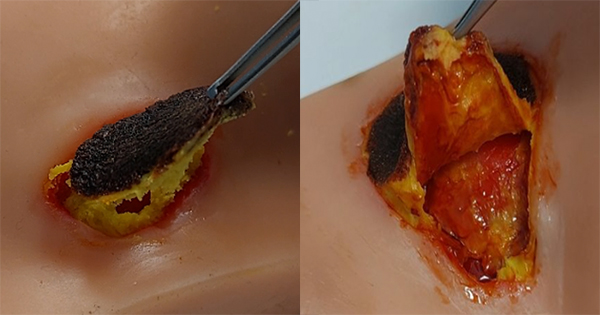
Debridement is considered beneficial in wound management as it addresses the cause of inflammation, optimises the condition of the wound bed, reduces the risk of infection and reveals the extent of tissue damage, enabling accurate wound assessment (Gray et al, 2010; All Wales Tissue Viability Nurse Forum, 2013; Strohal et al, 2013; Davies et al, 2015). In the UK, debridement often takes 3 months, by which time a wound is considered hard-to-heal (Wounds UK, 2016). Two previous debridement consensus statements support the use of larval debridement therapy (LDT) as a first-line option when speed, selectivity and bioburden are driving care decisions (Gray et al, 2010; Strohal et al, 2013). Literature and expert experience support the use of LDT as a rapid, selective, non-invasive treatment option for lower leg wounds, as a ‘stand-alone’ treatment or in conjunction with sharp debridement; however, this form of therapy is currently underused in practice despite being included on most formularies.
A panel of UK experts met in August 2019 to review the role of LDT in the management of lower limb wounds. They discussed the current treatment landscape, the benefits of LDT, possible barriers to its use, patient assessment and selection, and associated practical considerations. From their discussion, a treatment pathway has been devised that can be used by all members of the multidisciplinary team to inform the appropriate selection of LDT during clinical decision-making.
Purpose of this document
This document provides information and recommendations to support healthcare practitioners in the safe and effective prescription and delivery of LDT in practice, based on expert consensus. It focuses on lower limb wounds. The term ‘lower limb’ refers to any anatomical location below the knee, with wounds below the malleolus being sub-classified as foot wounds.
The evidence: Empirical versus clinical practice
At present there are no national guidelines on the use of LDT. There is currently a lack of empirical evidence, resulting from large blinded randomised controlled trials (RCTs), as it is difficult to blind patients to the use of larvae and there can be difficulties recruiting sufficient numbers of patients to generate statistically meaningful results (Dumville et al, 2009). Despite this, a large body of literature and anecdotal evidence from clinical practice support the use and benefits of LDT. This expert consensus serves to bridge the gap between empirical evidence and practice-based knowledge and experience.