This meeting report is based on a ‘Made Easy’ workshop that took place at the Wounds UK Annual Conference in Harrogate on 12 November 2024. The workshop and meeting report were sponsored by an educational grant from Flen Health.
Background
The number of people undergoing surgery is steadily increasing, with an estimated 313 million surgical procedures carried out each year worldwide (Meara et al, 2016). At the same time, the complexity of these procedures is also increasing. Each year, over 250,000 people in the UK undergo high-risk surgeries (Centre for Perioperative Care, 2020). The trend towards day surgery has further increased post-COVID-19, with NHS England setting a target for 85% of surgeries to be performed as day cases (NHS England, 2023). This shift has implications for the management of surgical wounds. Surgical wound dehiscence (SWD) often occurs after discharge, placing greater responsibility on primary and community services.
Surgical wounds are caused through surgical incisions and heal in two ways:
- Healing by primary intention: where wound edges are brought together and approximated.
- Healing by secondary intention: where tissue has been lost or wound edges cannot be brought into apposition for suturing, therefore healing must occur from the bottom of the wound upwards.
Surgical wounds are the most common type of wounds that require care within the NHS, with approximately 10 million occurring each year (Abbot et al, 2018). These complications include:
- Surgical site infection (SSI)
- SWD
- Seroma
- Haematoma
- Chronic wound development.
Scale of the problem
The estimated annual cost to the NHS for managing delayed healing in surgical wounds is £957.4 million–985.8 million (Guest et al, 2017). Surgical wounds account for 18.9–21.8% of total wound care expenditure, making them the most expensive to treat. The rate of SWD is estimated to range from 0.4–41.8% (World Union of Wound Healing Societies [WUWHS], 2018), while SSIs in the UK occur in approximately 0.4–11.3% of cases (UK Health Security Agency, 2022). It is worth noting that 60% of SSIs occur after discharge from hospital, which suggests that the true rate of SSIs may be underreported due to insufficient post-discharge surveillance (Anderson, 2018).
The full scale of surgical wound complications (SWCs) remains uncertain, partly because many cases of delayed healing go unrecorded. There is a lack of standardisation in the collection of post-discharge data, which limits the understanding of delayed healing after patients leave hospital. Moreover, it is unclear how many patients experience SWCs, as some may not return to the surgical team for follow-up care, especially if the complication is minor or the patient is discharged early.
Certain types of surgical procedures are associated with a higher risk of complications. These include cardiac surgeries (e.g. coronary bypass surgery), colon surgeries, hip and knee arthroplasties, abdominal and vaginal hysterectomies and vascular surgeries (e.g. aneurysm repair, thromboendarterectomy, and vein bypass). However, it is important to note that all surgeries carry some level of risk for wound complications, and any patient undergoing surgery may be affected.
Impact of SWCs on patients
The impact of SWCs extends beyond the physical aspects of healing. They can significantly affect a patient’s mental health, physical wellbeing and social functioning. Patients may experience pain, which may necessitate additional surgical interventions or multiple theatre episodes. Delays in discharge or hospital readmissions can extend the recovery process. In some cases, complications may lead to increased hospital and community visits and, in more severe cases, result in higher mortality, especially when infection is present. The financial impact on patients can also be substantial, as complications can delay their ability to work and cause long-lasting disability.
The impact on health and social care services is equally considerable. SWCs contribute to delayed discharges and increased lengths of hospital stay, hospital readmissions and additional surgical episodes. Elective surgery rates may also be affected due to these complications. Primary and community care teams experience a greater workload, particularly when managing the follow-up care for patients with complications. Dressing costs rise, and there may be an increased reliance on welfare and social security benefits due to prolonged disability. Furthermore, surgical wounds contribute to the growing problem of antimicrobial resistance (AMR).
Types of SWCs
SSI: Infection that develops after surgery in the part of the body where the surgical procedure was performed, typically within 30 days of the surgery, or 90 days if a prosthetic material was implanted during the procedure [Figures 1a–c].
SSIs are generally classified into three categories based on their depth [Figure 2]:
- Superficial: Affects skin and subcutaneous tissue
- Deep: Affects deeper soft tissue (e.g. fascia and muscle layers)
- Organs/Space: Affects any part of the body deeper than the fascia or muscle layer that was either opened or manipulated during a surgical procedure.
SWCs can increase the risk of SSIs, and conversely, SSIs can increase the risk of complications such as dehiscence. A dehisced surgical incision may or may not present with clinical signs and symptoms of infection. Similarly, not all infected or inflamed wounds dehisce (WUWHS, 2018). For more information on initiatives aimed at preventing and managing SSIs, see Box 1.
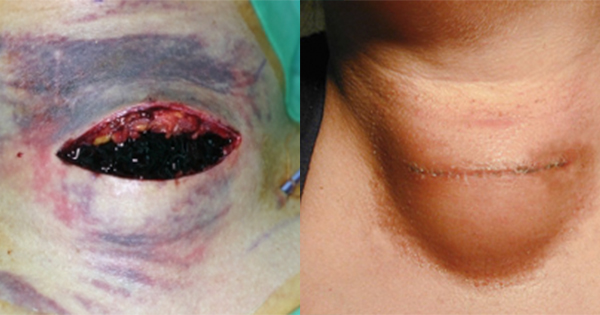
SWD: Separation of the margins of a closed surgical incision, which may occur with or without the exposure or protrusion of underlying tissue, organs or implants [Figure 3]. This separation may occur at one or multiple points along the incision, or may involve the full length of the incision. The extent of dehiscence determines whether it affects some or all layers of tissue.
Seroma: A pocket of clear serous fluid that develops after extensive surgical dissection, often as a result of the disruption of lymphatic channels. This fluid then leaks into a closed space, resulting in a collection of fluid. Diagnosis is primarily made through clinical examination, although it can be confirmed by needle aspiration or ultrasound if necessary. In most cases (approximately 90%), seromas will resorb on their own within six weeks and should generally be left to resolve naturally. However, symptomatic, persistent or infected seromas may require aspiration and drainage. Antibiotics should only be prescribed if an infection is suspected.
Haematoma: An abnormal collection of blood that can occur due to inadequate haemostasis during surgery or in patients who are anticoagulated or have abnormal clotting [Figure 4]. Diagnosis is typically made through clinical examination, with signs such as bloody wound drainage or an expanding mass. For small haematomas, treatment is usually supportive, with the expectation that the blood will be reabsorbed over time. However, larger haematomas or those that increase in size rapidly may require surgical evacuation, especially if the haematoma is located in critical areas such as the neck (where it could compromise the airway) or if the wound is in a contaminated area.
Several factors determine whether a wound will become infected, including:
- Host response
- Virulence factors of the pathogen
- Vascularity and health of tissue being invaded (including local ischaemia and systemic shock)
- Presence of dead or foreign tissue
- Prophylactic antibiotic use.
Prevention of SWCs
To minimise the risk of SWCs, all patients should be screened and optimised at the point of being listed for surgery (GIRFT, 2023). For every patient, except those undergoing emergency surgery, a pre-operative assessment must be carried out to identify potential risk factors and, where possible, address them before the surgery. If available, an objective, validated risk assessment tool should be used to enhance decision-making.
Pre-operative SSI prevention
For the prevention of SWCs, it is important to be aware of factors that can increase the risk of developing SSIs. Patient-related factors include:
- Age
- Nutritional status
- Diabetes
- Nicotine use
- Obesity
- Coexistent infection
- Altered immune response
- Long pre-operative stay.
- Pre- and intraoperative factors include:
- Inappropriate use of antimicrobial prophylaxis
- Infection at a remote site that is not treated prior to surgery
- Shaving the surgical site instead of clipping hair
- Long duration of surgery
- Improper skin preparation
- Improper surgical team hand antisepsis
- Inadequate environment of the room (ventilation, sterilisation of the operating room)
- Surgical attire and drapes
- Failure to maintain asepsis
- Surgical technique (e.g. haemostasias, maintaining a sterile field).
Pre-operatively, it is important to follow NICE guidelines for SSIs, which provide evidence-based recommendations aimed at reducing the risk of infection and promoting optimal outcomes for surgical patients. High-risk patients should also be considered for an Enhanced Recovery After Surgery (ERAS) programme. This programme, which targets the reduction of SWCs, is recommended for all patients undergoing surgery. While its adoption is not yet universal, documentation of its use is important to ensure that patients receive the most effective care.
A programme of prehabilitation should also be considered to optimise patients before surgery. This programme includes educating patients about expected wound outcomes, as well as the potential risks and benefits of the procedure. It is important to provide reassurance and manage patient expectations through education. Using pre-operative pathways should also be part of this process, to ensure that patients are fully prepared for surgery.
For clean surgery involving a prosthesis, clean-contaminated surgery or contaminated surgery, prophylactic antibiotics should be administered. For dirty surgery, antibiotics are required for both treatment of existing infection and prophylaxis against further infection. An active wound care strategy should accompany antibiotic therapy to optimise wound management. Routine hair removal should be avoided. If necessary, it should only be performed immediately before surgery using electric clippers.
Intra-operative SSI prevention
Before making the incision, the skin at the surgical site should be prepared with an antiseptic solution. Chlorhexidine has been shown to be more effective than Betadine for skin preparation; however, it is important to check for any potential allergies to chlorhexidine beforehand, as some patients may have sensitivities.
If gloves or gowns become contaminated, they must be changed. Wound irrigation should be performed at the closure stage and careful attention should be given to surgical techniques. The method of wound closure should be selected based on the specific procedure and patient needs.
Post-operative SSI prevention
Wounds should be closely monitored after surgery, particularly those in areas prone to complications, such as skin creases and under skin folds (e.g. the groin).
As important as it is to educate patients before surgery, it is equally important to ensure they are informed about how to protect and support their wounds after surgery. Patients should be guided on managing activities such as coughing, vomiting or sneezing to avoid strain on the surgical site. To prevent or reduce oedema, elevation should be encouraged where appropriate.
Patients and their carers should be made aware of the risks associated with surgery and the signs and symptoms to monitor [Box 2]. This includes recognising signs of dehiscence. Supporting self-care and advising patients to avoid excessive stress on the incision is important. Patients should also follow activity guidelines, such as avoiding returning to work too soon or lifting heavy objects.
Early SWCs
Early SWCs include but are not limited to, haemorrhage and catastrophic dehiscence (known as burst abdomen), which may require immediate intervention to prevent further harm.
When early complications are detected, it is important to treat the situation as an emergency:
- Call for help
- Lay the patient flat to reduce blood pressure
- Apply a clean or sterile dressing to the bleeding site
- Maintain direct pressure to the wound site until medical assistance arrives
In some cases, vertical or horizontal deep tension sutures [Figure 5] may be required to help prevent wound dehiscence, particularly in high-risk patients, such as people with obesity.
Catastrophic dehiscence
In the case of a catastrophic dehiscence, there is a separation of the surgical incision, potentially exposing internal organs or tissues. It is important to immediately inform the surgical team and ensure the patient is stabilised for transfer to theatre as necessary.
If the dehiscence is severe enough to expose the bowel [Figure 6], it is considered a major complication and requires urgent intervention. The exposed viscera/organs should be covered with saline-soaked gauze until the patient can be taken to the theatre. The saline-soaked gauze should then be changed hourly to prevent desiccation of viable tissue.
If the dehiscence is less severe, with the bowel remaining inside, it is considered a minor complication. Although less critical, this situation still requires urgent attention to prevent further complications and ensure appropriate management. If the patient has been discharged and experiences these symptoms, emergency services should be contacted.
Intermediate SWCs
In addition to early complications, there are intermediate complications, such as sepsis and cellulitis, which may develop after surgery and require urgent medical attention.
Sepsis, which is a sign of systemic infection that can spread throughout the body, is a particular concern and requires quick identification and management. Systemic signs of infection, such as fever, increased heart rate and altered mental status, should prompt an immediate review by a senior clinician. Local guidelines and NICE (2024) guidelines for managing sepsis should be followed.
Cellulitis (also known as a spreading infection) occurs when bacteria and/or their products invade surrounding tissues, causing diffuse, acute inflammation and infection of the skin or subcutaneous tissues. It may develop at the surgical site and requires immediate treatment with antibiotics (International Wound Infection Institute, 2016).
However, due to the rise of AMR, it is important to delay the administration of antibiotics until microbiological results are available, where possible.
Local signs of infection, such as erythema, swelling, pain, pus and heat, or dehiscence in cases involving surgical implants (e.g. mesh, prostheses or an exposed implant), should also be closely monitored. If these signs are present, an immediate review by a senior clinical decision-maker should be arranged, ideally within 24 hours.
Further complications requiring immediate referral
There are certain complications that require referral to the surgical team within a defined time frame, typically within 72 hours. These include dehiscence with exposed subcutaneous layers and fascia, suspected sinus or fistula formation, draining seromas or haematomas, enterocutaneous fistulas and peri-stoma wound dehiscence. It is important to refer these cases to the surgical team as quickly as possible to prevent further complications and ensure appropriate management.
While these complications can occur in both hospital and community settings, patients who are at higher risk of SWCs are more likely to be managed in a hospital rather than a community setting. This is particularly true for patients undergoing complex or high-risk surgeries, where the likelihood of complications is higher.
Complications in hospital versus community settings
Hospital setting: In a hospital setting, patients are often at higher risk due to the complexity of their surgeries, which increases the likelihood of developing complications. Surgeon-related factors, particularly in the acute postoperative period, play a significant role. Early complications, such as haemorrhage, catastrophic dehiscence, or the formation of haematomas and seromas, are more commonly observed in this environment. These complications typically manifest within the initial days following surgery and require immediate identification and management.
In hospital settings, it is important to regularly observe the surgical closure site for any signs of bleeding or swelling. Close attention should be paid to whether the closure method is intact, ensuring there is no compromise at the incision site, such as the suture cutting into the skin or through it.
Community setting: In contrast, the community setting tends to present with complications at a later stage in the post-operative process. Wound infections typically develop around days 4–5, presenting with signs like heat, redness, swelling and pain. Dehiscence in the community is often linked to patient factors, such as comorbidities, rather than surgical technique.
The majority of haematomas and seromas occur later and will be reabsorbed over several weeks. Dehiscence in the community usually begins as a small opening in the wound but can progressively grow over days 4–9. Any swelling, oozing beyond day 5, broken clips or sutures, and any sudden increases in pain, may indicate emerging complications.
What is the difference between inflammation and infection?
Inflammation is a normal part of the healing process. Typically, it manifests as swelling, heat and pain, and can occur even if the wound is not infected.
In contrast, infection occurs when pathogenic microorganisms, such as bacteria, enter the body and begin to multiply. Clinical signs of infection (e.g. swelling, heat and pain) overlap with those of inflammation. However, while inflammation will almost always occur when infection is present, it is possible to have inflammation without infection.
If infection is suspected, immediate action should be taken, such as:
- Sending discharging fluid for:
- Gram staining
- Culture and sensitivity testing (a culture swab of a wound should only be taken if clinical infection is suspected; it is important to differentiate between a wound being infected versus contaminated).
- Initiating broad-spectrum antibiotics until culture results are available.
The action of treatment will depend on the severity and timing of the infection. For more severe cases, immediate steps should be taken to open and debride the wound thoroughly. It is often better to debride a wound than to wait for antibiotics to take effect. Depending on the nature of the wound, resuturing may be necessary, or the wound may be managed as an open wound, with the use of antimicrobial dressings as appropriate.
It is important to recognise and differentiate between inflammation and local infection, as this helps avoid the overuse of antibiotics or topical antimicrobial treatments. Erythema has traditionally been used to detect skin areas that may be infected or have other abnormalities. Although the term ‘redness’ may be used, it is important to note that erythema does not always appear as redness in many skin tones. While redness can be an obvious symptom in people with less deeply pigmented skin, where it contrasts clearly against light skin tones, this is not necessarily the case in people with varying skin tones; e.g. black, brown and olive skin tones. Changes in colour can run the spectrum of pink, red and purple and in some cases it may be limited to a subtle darkening of the existing skin tone (Wounds UK, 2021; Dhoonmoon et al, 2023). Additional care or techniques may be needed for accurate diagnosis.
SWD
The occurrence of SWD following different surgical procedures has been reported as ranging between 1.3% and 9.3% (Sandy-Hodgetts et al, 2015). Although SWD can occur at any time following surgery, it generally occurs 4–14 days after surgery (WUWHS, 2018). If SWD occurs early (within the first 24–48 hours), patients will need to return to theatre for resuturing. However, in some cases, managing the condition with dressings and negative pressure wound therapy (NPWT) may be appropriate.
Signs of SWD include:
- Inflammation beyond normal healing (typically after day 5).
- Swelling, oedema, seroma, redness, bleeding and/or exudate at the incision site.
- Opposed suture margins opening or separating at any point along the incision .
- Broken sutures or clips.
- Pain at the incision site.
- A “popping” sensation during activities that increase intra-abdominal pressure (e.g. straining or coughing).
SWD may occur due to:
- Technical factors: Issues with the closure of the incision (e.g. choice of thread, structures in the wound incision and suture technique – knotting or stretching of sutures)
- Mechanical stress: Excessive mechanical stress, force or swelling placed on the incision (e.g. oedema, abrupt or vigorous movement, falls, straining, coughing spells, vomiting, physical trauma or pressure from haematoma or stoma)
- Disrupted healing: Caused by a combination of local and systemic factors [Box 3] (Sandy-Hodgetts et al, 2013, 2018; WUWHS, 2018; Gomes et al, 2020).
Assessment of SWD
A holistic assessment is important to identify contributing factors and manage the condition effectively. Key aspects include:
- Recording events leading to dehiscence (e.g. vomiting, coughing).
- Wound assessment (e.g. wound classification, approximation of wound edges, crepitus, healing ridge, fluid collection and areas of dehiscence).
- Documenting details about the surgery (e.g. type of procedure, timing, emergency or elective status, closure materials and date of removal, and the presence of drains, prosthesis or implants).
Assess each area of dehiscence individually and consider using a grading system to classify the severity and help understand and describe the findings. Examples of grading tools for SWD include the WUWHS Sandy Grading Tool and the T.I.M.E Clinical Decision Support Tool.
Treatment
SWD can be frightening for patients. It is important to provide reassurance, manage their expectations, and educate them about the condition. Pain management should be prioritised, and efforts should be made to remove or reduce any contributing risk factors. For example, if a patient has developed SWD due to persistent coughing caused by a chest infection, treating the underlying chest infection can help mitigate the issue.
The local management of dehisced wounds depends on:
- Severity and depth.
- Presence of infection.
- Timing of dehiscence.
- Presence of comorbidities.
Flaminal®
Flaminal® is a primary dressing and autolytic debridement solution suitable for various wound types, including post-surgical wounds. Its triple mode of action avoids the need for multiple products and make it suitable for a variety of wounds and tissue types:
- Debriding gel: Flaminal® continuously debrides the wound (Flen Health, IFU).
- Absorbent alginate: Flaminal® absorbs excess exudate (Flen Health, IFU).
- Antimicrobial enzyme system: Flaminal® offers antimicrobial protection and reduces bacteria released from biofilm (De Smet et al 2009; Cooper, 2013).
Flaminal® in practice: case study
The session continued by highlighting the role of Flaminal® in practice [Box 4], using the case of a 56-year-old patient who underwent breast cancer surgery and accompanying reconstruction.
Antimicrobial resistance
AMR is a growing global concern, exacerbated by the widespread and inappropriate use of antimicrobials. This misuse has significantly contributed to the rise of AMR, with an estimated 10 million deaths annually projected by 2050 if no action is taken (Interagency Coordinating Group on Antimicrobial Resistance, 2019).
SWCs play a role in the development of AMR through increased antibiotic use, including misuse and overuse, which allows bacteria to develop resistance mechanisms. Invasive procedures, such as abscess drainage, heighten the risk of resistant bacteria entering wounds, while prolonged hospital stays increase exposure to healthcare-associated infections and resistant pathogens. Additionally, biofilm formation in infected surgical wounds can lead to persistent infections, necessitating prolonged antibiotic treatment. Inadequate infection control practices and cross-contamination of equipment further facilitate the transfer of resistant pathogens between patients, compounding the problem.
Implications of AMR
The implications of AMR extend beyond patient care. The increased incidence of resistant infections contributes to a greater workload for healthcare providers and community services. Limited education on infection management, a lack of structured assessment tools, and inadequate referral pathways to surgical teams can affect the quality of care. Additionally, the need for extended treatment and additional interventions may result in higher healthcare costs. To address these challenges, it is important to promote antibiotic stewardship, enhance educational initiatives for practitioners, and use innovative antimicrobial wound care alternatives, such as Flaminal®, which shows no cytotoxicity.
Delegate responses
During the ‘Made Easy’ workshop, delegates were asked a range of questions [Box 5]. At the beginning of the workshop, only 23% of attendees felt confident in identifying and managing different types of SWCs, with 5% expressing no confidence. By the end of the workshop, confidence levels had significantly improved, with 52% reporting confidence and none lacking it.
However, the responses also highlighted challenges in SWC management. A majority (72%) believe that SWCs have increased since COVID-19, yet only 17% have a structured pathway or algorithm for managing these complications, and just 21% use a dedicated surgical wound assessment chart.
These findings indicate that while the workshop successfully improved knowledge and confidence, there remains a need for greater adoption of structured tools and resources to standardise surgical wound care practices.
Key messages
The ‘Made Easy’ workshop provided practical guidance on SWCs and highlighted the following key points:
- Not all SWD is caused by infection.
- The majority of SWCs occur post-discharge.
- SWCs are under-reported.
- The increased volume of SWCs is impacting community healthcare workloads.
- Education is needed to make staff aware of the signs and symptoms to promote early intervention and reduce severity.
- Pathways for referring patients back to the surgical team need improvement.
- SWCs can contribute to the development of AMR.