The other major change is that the limitation on the number of hours of simulated learning has been reviewed meaning that AEIs can now include 600 hours of simulation-based activities, which sees the previous cap doubled. Certainly, the COVID-19 pandemic saw universities and institutions having to develop more resources for simulated clinical skills and many have been able to invest in the technology and assets needed to ensure the learning experience reflects clinical practice. But what about those AEIs who don’t have the necessary budget and trained staff to take this forward, how will they be supported?
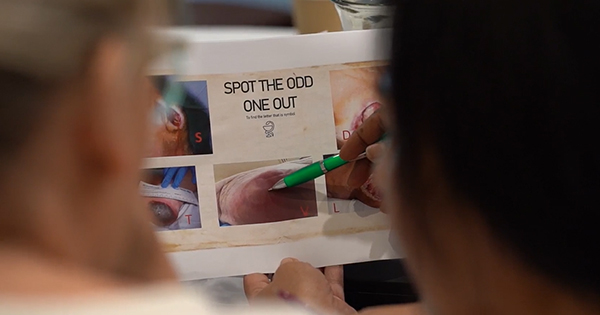
While there will certainly be challenges in realising the move to more simulation-based activities it does provide an opportunity for AEIs to work more closely with specialists working in clinical practice many of whom have been using simulation skills in their teaching. Indeed, in terms of wound management there have been published examples over the last eight years of the use of Telemedicine for student nurses (Christiansen and Rethmeier 2015), clinical simulation to teach wound evaluation and treatment (Silva et al, 2020) and simulated wound care to assess competence (Kielo-Viljamaa et al, 2021). I’m also aware from attending various UK and European conferences that there are many more innovative examples of the use of simulation for teaching and assessing wound care related skills. It would be good to share those examples so that AEIs can tap into the creative wealth of experience that is already out there. The change also provides opportunities for tech-based companies to work with AEIs and clinicians to ensure that simulations reflect the real world of clinical practice. Importantly, what we don’t want to do is lose the person-centred approach to providing care, therefore provision of wound care in a simulated way needs to embed the wider context of effective communication skills and empathy in particular. Simulated learning also needs to be able to reflect the nuances of caring for different populations for example providing wound care in an older person with dementia or treating an individual with a hearing impairment.
For those of you working in an AEI what are your thoughts on the changes to the education standards, what are the implications for your institution? It would also be good to hear from those colleagues working in AEIs with a specific responsibility for simulated learning, is the flexibility to include more hours in the curriculum welcomed? Finally, but as important, what are student nurses thoughts on the potential for more simulated learning, specifically for wound management? Have you got some good examples of how this has enhanced your learning and prepared you for treating wounds in-person?
You can email your comments to the Editor: Rachel Webb @rwebb@omniamed.com.