In January 2022, I was appointed as a tissue viability nurse (TVN) and later promoted to tissue viability (TV) matron in February 2023 at the North Bristol Trust (Bristol, UK). Prior to this, I held various roles in social care, including lead community nurse, the clinical lead for one of the largest UK care home providers. I worked in complex care within social care, delivering continuing healthcare. I also served as a registered Care quality commission manager for a care home. My interest in wound care has been a consistent focus, even during my time as a student nurse.
As a community nurse, I often found it difficult to understand why patients with leg ulcers were admitted to primary care, only for their treatment – compression bandaging – to be discontinued. When I started my role as a TVN at the North Bristol Trust, I encountered similar concerns from patients and their families. They voiced frustration and confusion about why compression bandaging was halted after so much effort had been dedicated to healing their leg ulcers prior to admission.
Background
Historically, acute hospitals have had a limited role in diagnosing and treating patients with leg ulcers, and predominantly, community care settings have delivered this care. Upon hospital admission, it has been standard practice to remove compression therapy and discontinue until the patient is discharged back to community care. Investigations into the aetiology of leg ulcers are rarely undertaken for inpatients, leading to inconsistent management of patients with leg ulcers, which can potentially delay healing. Driven by the national agenda to change the approach to leg ulcer care, the TV team was frustrated with the inequality of leg ulcer care across the whole health system.
Assessing the impact of the issue and the number of patients admitted with leg ulcers was challenging due to limited hospital data. It was estimated that approximately 180 patients per month attended the hospital with an unspecified leg wound.
In order to address this, the hospital trust TV team established collaborative leg ulcer pathways and a virtual clinic to ensure continuity of care for patients whilst in hospital.
Methods
The TV team received referrals from hospital ward staff seeking advice on managing venous leg ulcers. The wound care guidance provided typically included recommendations for an appropriate primary dressing, a secondary absorbent dressing, followed by wadding and crepe bandaging.
However, according to evidence-based practice and the National Wound Care Strategy Programme recommendations (National Wound Care Strategy Programme, 2022; National Institute for Health and Care Excellence, 2024), a full lower limb assessment should be conducted, and compression bandaging should be applied if appropriate. Therefore, offering advice that did not align with these guidelines seemed inadequate.
Despite this, the TV team had limited knowledge and skills in assessing and managing leg ulcers. Additionally, concerns were raised by ward sisters, staff, and the vascular team regarding the application of compression bandaging for venous leg ulcer patients in the hospital. The primary concern was the risk of patients developing deep tissue injuries to the heel under the bandage. There was also uncertainty about whether compression bandaging was necessary in the hospital setting, as patients would be in bed, and this would negate the need for compression bandaging.
The North Bristol Trust TVNs collaborated with Urgo Medicaland their clinical specialist to develop a lower limb pathway that mirrors the community pathway, supporting continuity of care between community and acute providers. The TVN team also explored the use of wraps and compression stockings, as is common practice in the community. However, this posed a challenge in the hospital setting, as there was no facility to launder the garments, and patients had to rely on relatives or friends for this support. The use of wraps and stockings was discounted unless the patient was admitted with them in situ and wanted to continue to use them with family support during their inpatient stay, if clinically appropriate.
In consultation with our vascular consultants and nurses involved in the collaborative leg ulcer pathway, it was recommended that the toe–brachial pressure index be used instead of the ankle–brachial pressure index. This recommendation was adopted and implemented.
The TVNs received education on lower limb assessment, including practical workshops and competency sign-off for compression bandage application, delivered by the Urgo clinical specialist. They also engaged with the North Bristol Trust vascular scientists who conduct lower limb vascular assessments for inpatients. Although there were initial concerns about the potential increase in workload for the vascular team, the initiative was ultimately supported by them. There was engagement and education in the admission wards and the inpatient wards on the respective leg ulcer pathway applicable to the clinical area.
There were no additional resources allocated for the implementation of this project. However, clinical support was provided by the Urgo clinical specialist through an honorary contract. The TV team also benefited from recently increased clinical capacity, made possible by streamlining processes related to electronic referrals, documentation and incident investigations.
From inception to implementation of the project was approximately 1 year.
Collaborative working with stakeholders enabled the creation of two leg ulcer pathways, enabling seamless care for patients in hospital and community services [Supplementary Material]. Separate pathways were developed for admission areas and hospital wards to standardise leg ulcer care prior to attending the virtual clinic.
- A virtual leg ulcer clinic was established, allowing ward staff to submit electronic referrals. In addition, the TV team introduced a dedicated inpatient leg ulcer round, during which they deliver specialised care directly to patients with leg ulcers.
- Standardisation of product choice – a two-layer multi-component bandage system and a Technology Lipido-Colloid nano-oligosaccharide factor contact wound dressing were implemented as the first choices for those with complex leg ulcers
- Partnership working with industry and community TV team to provide education and clinical skills training to the TV team, and support pathway development.
Results
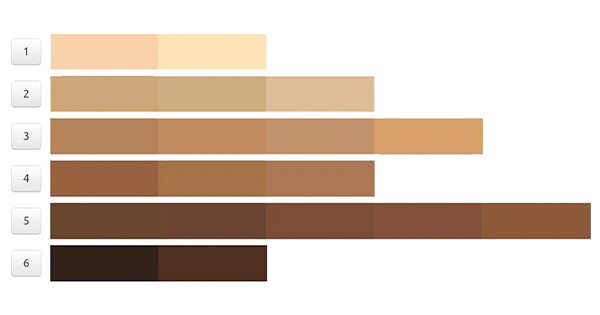
The leg ulcer virtual clinic opened for referrals in April 2024. In the first 8 months, 146 patients were reviewed by the service; 35% of these patients had not had an ankle–brachial pressure index completed prior to admission, and 34% patients were not in compression therapy before admission. A total of 51% of patients admitted for compression therapy were receiving full or reduced multi-component bandaging, with the remaining 14% receiving compression wraps, short stretch bandages or hosiery [Figure 1].
Patients referred to the virtual leg ulcer clinic were reviewed virtually on the next working day. Wound care recommendations were provided to the clinical and nursing teams, including referrals to the vascular scientists when appropriate. Patients were then seen face-to-face within 7 days by a TVN for a full lower limb assessment.
Upon discharge from the North Bristol Trust, the TVNs communicated the lower limb wound management plan to the relevant community, practice, or social care teams to ensure continuity of care. However, assessing the impact of the lower limb pathway on venous leg ulcer healing has been challenging due to time constraints, governance on data protection and the use of different IT systems across organisations.
A positive response has been received from patients who have had their compression therapy continued whilst in hospital. The TV team has enjoyed learning and developing new skills and knowledge, enabling them to provide seamless leg ulcer care for patients, and the introduction of the ward and admission area pathways has given the nurses confidence in managing patients with leg ulcers.
The TVNs submitted feedback after implementing the lower limb pathway and completing team training:
- “My confidence in assessing and managing leg ulceration has improved since we embarked on the leg ulcer project.”
- “It has been really exciting learning a new skill that will benefit our patients.“
Discussion
It was difficult to obtain accurate data on the number of admissions with a lower leg wound. As a team, we decided that we would start lower leg wound assessments and compression bandaging in line with the National Wound Care Strategy Programme recommendations. Due to the short length of stay and medical reasons for admission, such as decompensated heart failure and cellulitis, for inpatients, it is not always appropriate to commence compression bandaging. However, we can advise on vascular investigations to support wound management on discharge, so support the clinical team.
Initiating the service has had its challenges. Securing project funding in the current NHS climate has been difficult. Ward clinicians were concerned about the potential increase in pressure damage to heels concealed within the bandages, so robust management plans were provided to these areas, and managing care for patients in bed has presented difficulties with bandage application and manual handling. Where possible, patients are encouraged to sit out of bed for their leg ulcer care, and manual handling advice is sought where required. Maintaining compression therapy for patients discharged on the rehabilitation pathway through private providers, such as care homes, was also problematic. The project has initiated a health system-wide drive to improve lower limb care for patients, which has motivated other local acute trusts to consider service change for patients. Awareness of the importance of continuity in leg ulcer provision was raised with the Integrated Care Board and at a local wound conference. Collaborative working has led to the development of a lower limb assessment and referral pathway across primary and acute care, including a vascular intervention referral process. A digital wound care solution for lower limb wounds, including diabetic foot wounds, is being created, which will produce robust data and track patients across primary and acute care.
Conclusion
Challenging the status quo of patient care delivery requires drive, determination, and courage. The TV team identified that the lack of consistent leg ulcer care within acute care was impacting patients and that there were system-wide inconsistencies. By working collaboratively with a range of stakeholders, they have commenced a journey to improve leg ulcer care further across their area.
Next steps
The implementation of a lower limb pathway and compression bandaging therapy has revealed additional challenges within the healthcare system in delivering effective, evidence-based therapeutic care for patients with leg ulcers across organisations. In response to these challenges, the North Bristol Trust TVN team has introduced a MESI toe–brachial pressure index machine to enhance lower limb assessments for inpatients with leg ulcers.
The culture within the North Bristol Trust has evolved, with increased awareness of the role of compression bandaging in managing venous leg ulcers. This has led to more referrals from clinical and nursing teams specifically for compression bandaging. It is recognised, however, that the TVN team cannot manage all lower limb compression needs within the North Bristol Trust. To address this, vascular ward nursing staff will be educated and trained to become clinically competent in the application of compression bandaging. This initiative is currently being treated as a pilot project, with the intention of expanding it to include care of the elderly wards in the future.
The team is also reviewing strategies to improve discharge processes through strengthened communication with community nursing teams, primary care providers, and social care services.