Pressure ulcers are common, complex wounds affecting people across different populations and care settings (Shi et al, 2019). They continue to be one of the top 10 patient harms in England and, as such, reducing pressure ulcers continues to be a national focus (Fletcher 2022). The negative impact on patients and their families is widely recognised. Reducing the prevalence of pressure ulcers contributes to improvements in health outcomes, quality of life, length of stay, and minimises pain and suffering for patients. In turn, pressure ulcer reduction has positive financial implications for organisations, avoiding extensive treatment costs and costs associated with potential litigation.
The National Institute for Health and Care Excellence (NICE) states that using pressure-relieving and pressure redistributing devices is a widely accepted approach to preventing pressure ulcer development in people assessed as being at risk (NICE, 2014). The devices, which include mattresses, overlays, cushions, and seating, work by reducing or redistributing pressure, friction, or shearing forces. It is recognised that these devices should be used in conjunction with other preventative strategies, such as repositioning.
The choice of device can depend on patient factors, such as their mobility or skin status (NICE 2014), but of course, in practice, it will also depend on what equipment is available and accessible within an organisation.
Shi et al (2019) explain how different pressure redistribution surfaces aim to redistribute pressure, to increase blood flow to tissues, and relieve skin and soft tissue deformation. Active surfaces work by regularly changing the points of body contact with the mattress, reducing the time pressure is applied to specific anatomical sites. Reactive surfaces work differently. Their action is passive and includes immersion (or sinking of the body into the surface) and envelopment (where the surface conforms to the body). They spread the pressure over a larger surface area and achieve lower pressures at specific sites on the body. Low air loss surfaces also aim to improve the skin microclimate to maintain skin and tissue integrity, which can be particularly useful in people with incontinence. The review concluded that compared with foam surfaces, reactive air surfaces may reduce pressure ulcer risk and may increase pressure ulcer healing; however, it noted that more high-quality research is still needed to compare reactive air surfaces with alternating pressure air surfaces, for example (Shi et al, 2019).
Blackburn et al (2024) stated that despite recommendations to use pressure-redistributing mattresses, the evidence is still inconclusive about the most effective type of surface and the benefits for pressure ulcer prevention and management, and for patient comfort. The cost-effectiveness of these devices also requires further study. To support a better understanding of how these devices can contribute to pressure ulcer prevention and management, they stated that further research should focus on a standardised approach to measuring patient outcomes.
About Dolphin Therapy
Dolphin Therapy (Medstrom) was originally created by US naval engineers to prevent crushing injuries to dolphins during transportation. It has undertaken a remarkable journey and is now one of the leading surface technologies for pressure ulcer prevention and treatment in the most complex patients. It provides a step up from a dynamic active mattress. This surface has been evidenced to deliver outstanding outcomes for those at highest risk of developing pressure ulcers. The Dolphin Therapy system is shown in Figure 1.
Clinicians at Liverpool Heart and Chest Hospital (LHCH) observed that patients who had been on the theatre table for an extended period often developed higher category pressure ulcers. In addition, some patients cannot be repositioned postoperatively, due to haemodynamic instability, or because their chest is left open after cardiac surgery. As a result, full repositioning is not possible, which can be for several days. These circumstances posed a significant challenge in preventing pressure ulcer development.
As part of the overall Trust strategy to reduce pressure ulcer incidence, LHCH worked in partnership with Medstrom to provide the highest specification products to the highest risk patients at the very earliest opportunity. In 2014, the Trust first trialled Medstrom’s Dolphin Therapy, a reactive system that creates a simulated fluid environment to fully immerse patients whilst optimising pressure redistribution, maintaining tissue symmetry and maximising tissue oxygenation. After successful outcomes were recorded, it was identified that acute postoperative patients could be nursed proactively on Dolphin Therapy to help prevent pressure ulcers from developing.
A business case was compiled for the proactive use of the unique support surface, as well as defining a set of patient selection criteria to support appropriate use, including:
- Patients who have been in the cardiothoracic theatre for more than 16 hours
- Patients who will have an open chest postoperatively
- Patients known to be too unstable to be repositioned postoperatively.
- Patients who have returned to theatre for re-sternotomy/exploration.
Due to the success of Dolphin Therapy in reducing pressure ulcer incidence, this criteria was extended to include patients with existing sacral pressure ulcers, of category 2 or above.
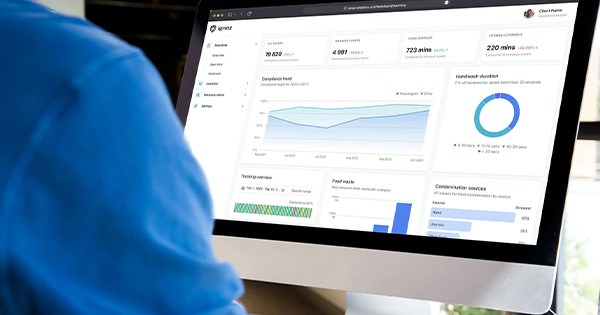
Fundamental to the partnership between Medstrom and the Tissue Viability Service (TVS) has been the deployment of a Medstrom clinical advisor for weekly visits. The role of the clinical advisor is to offer clinical support and guidance on appropriate patient use, since Dolphin Therapy is not required for every patient. Adherence to the protocol is regularly reviewed, with data presented to the TVS. This is key to the valued partnership working between Medstrom and LHCH.
Both organisations have a shared vision for appropriate patient use, which is seen by the effective step-up and step-down of patients based on regular clinical assessment. In addition, the collection of patient outcomes via the clinical advisor is fundamental to us being able to justify the value that Dolphin Therapy brings, as originally outlined in the business case.
Patient outcome data
Since January 2022, Medstrom, in partnership with LHCH, has made the effort to follow the journey of every patient being placed on a Dolphin Therapy mattress. Details before placement are collected, including their initial status as a prevention or treatment patient, all relevant comorbidities, skin status and their overall clinical objectives. The journey is then finalised by collating their outcomes after placement on Dolphin Therapy and since 2022, 697 individual patient outcomes have been collected.
The evidence highlights the complexity of the those nursed on Dolphin Therapy, with 88.83% identified as being very high risk of pressure ulcer development, accompanied by various clinical conditions ranging from cardiovascular and neurological through to respiratory and musculoskeletal.
Of the patients, 97.5% (n=585) were assessed as being high or very high risk, using the Waterlow Risk Assessment Tool, and 2.5% (n=15) medium risk [Figure 2]. Dolphin Therapy was used for pressure ulcer prevention in 87.5% (n=525) and for treatment in 12.5% (n=75) [Figure 3].
The proactive approach adopted by the Trust is reflected in the fact that 87.5% (n=525) of patients did not have existing skin damage when placed on Dolphin Therapy, and therefore staff had selected Dolphin Therapy for prevention purposes. Remarkably, none of these patients acquired new skin damage; therefore, Dolphin Therapy was 100% effective at preventing skin damage, improving patient safety for this complex postoperative patient cohort [Figure 4].
Dolphin’s efficacy and impact on patient safety is also evident for those treatment patients, almost 12.5% (n=75). In this treatment group, pressure ulcer categories included categories 2 and 3; 20.99% fully healed, 50.62% improved and 28.39% remained static and 0% deteriorated during their in-patient stay [Figure 5].
The introduction of the Patient Selection Criteria and Ordering Document has been critical to maintain best practice throughout the organisation and appropriate use maintained. As the Trust’s experience of using the Dolphin Therapy surface has grown, further patient criteria have been identified and updated on the document. Significant additions include:
Patients with non-resolving non-blanching erythema to the sacrum. This is one of most commonly occurring anatomical sites for pressure ulcer development. The tissue viability nurses (TVNs) observed that following transfer of these patients to Dolphin Therapy, the non-blanching erythema quickly resolved.
Patients who have had an out-of-hospital cardiac arrest. Dolphin Therapy has been successful in the support of these patients who can often experience ‘long lies’, whereby they have been lying on a hard surface for a prolonged period. When they arrive, they may initially be too unstable to fully reposition, so their “welcoming” surface is Dolphin Therapy. This continues with them as part of their tissue recovery and their overall pressure ulcer prevention plan.
LHCH is not the only organisation using the fluid immersion simulation system to realise outstanding benefits for complex patient care. Dolphin Therapy is used by healthcare organisations across the UK and Ireland, with data to showcase almost 7,000 patient outcomes for the product nationally.
Given that timely access to Dolphin Therapy was critical to proactive placement of patients, LHCH had ‘Medstrom Now’ lockers installed. These allow several units to be stored on site, so they are accessible by staff at all hours. The unique and ethical rental solution eliminated the time and cost associated with ad hoc delivery, allowing placement on the surface to meet the needs of emergency patients.
Additionally, staff involvement has been integral for ensuring this process, alongside acknowledging the patient criteria and appropriate use of Dolphin Therapy, is maintained. Ongoing staff education and training is delivered via Medstrom’s Clinical Advisor, working closely with clinicians to ensure they understand the benefits to the patient and the necessary time for step-up and step-down to/from the high specification surface.
Staff feedback remains positive regarding the impact of early adoption of Dolphin Therapy on patients and staff alike. A tissue viability specialist nurse at LHCH observed first-hand how it has improved patient outcomes. Her background before becoming a TVN was in critical care, which is where she first saw the Dolphin in effect. Afterwards, she stated that she saw a huge change — critical care staff noticed that the number of pressure ulcers reduced, and patients’ skin integrity improved. She commented that it is an easy product to use too, so the transition for the staff was easy.
The positive impact on patients has also been well documented. One patient placed on the Dolphin for the treatment of existing pressure ulcers, said: “I can honestly say, the Dolphin Therapy mattress has been very comfortable. I’ve had several pressure ulcers, as well as severe oedema, and it’s really helped with those symptoms. In fact, I’ve been able to overcome them and today, the pressure ulcers are completely healed.”
The outcomes seen in LHCH demonstrate that Dolphin Therapy is an effective strategy for reducing the risk of hospital-acquired pressure ulcers. It is part of our preventative strategy, rather than being reactive after pressure ulcers have occurred. We continue to collect outcome data for patients, while striving to follow-up and enhance the data further based on those discharged. We would suggest other organisations move forward with their own evaluations to see if Dolphin Therapy can improve patient outcomes as it has done for us.
The partnership between LHCH and Medstrom can demonstrate value in numerous different ways. Notably, the most important value is seen via the improved safety and care provided to those patients deemed at high risk of developing pressure ulcers. Pressure ulcers are still considered a largely preventable harm associated with healthcare delivery, therefore when able to be prevented this provides an enormous value to patients in terms of their hospital experience and beyond.
When factoring in objectives additional to pressure ulcer prevention and treatment, the holistic value can also be evidenced. For all patients who had specific objectives relating to outcomes such as improvement in comfort (60), pain management (26), reduced turning (365) or sleep (15), 100% of those objectives were either fully or partially met for each category [Figure 6]. This contributes to improved patient experience, promoting dignified care that equally has a significant impact on caregiver and family wellbeing too.
The treatment of pressure ulcers costs the NHS more than £3.8 million every day, while one hospital-acquired pressure ulcer increases a patient’s length of stay by 5-8 days, on average (NHS Improvement, 2018; Labau 2020).
By using the pressure ulcer productivity calculator (Department of Health and Social Care, 2010), the financial value to the Trust in terms of pressure ulcer prevention, a more specific cost can be calculated. For example, a total of 350 pressure ulcers being treated a year, split between categories 1 to 4, can equate to a treatment cost over £2 million. If only a quarter of these pressure ulcers were prevented, savings would equate to £510,000 per year. This can be a powerful tool to justify expenditure on effective pressure ulcer prevention strategies, such as pressure-redistributing mattresses.
Conclusion
While other contributing factors should be considered, the contribution to pressure ulcer prevention evidenced by Dolphin Therapy affords significant financial savings. In turn, these financial savings spread beyond just pressure ulcers, supporting improved patient flow and earlier rehabilitation and discharge, and contribute to a safer patient environment and an improved patient experience.