A 78-year-old gentleman named Barry contacted his GP with a history of a sudden onset of ulceration to his left lower limb with no recall of any trauma to this area. The GP arranged for him to be assessed by the practice nurse in the leg ulcer clinic.
The nurse undertook a holistic patient assessment. Barry had hypertension, congestive cardiac failure, angina, and hyperthyroidism. Medication included Bricanyl, Duoresp, GTN, paracetamol, cosmocol, salivix pastilles, alfacalcidol, aspirin, candesartan, digoxin, frusemide, levothyroxine, lansoprazole and Nicorandil.
A wound assessment and vascular assessment were also performed. His ABPI following doppler was 1.1 mmhg and his pedal pulses were palpable and biphasic. His limb and foot were well perfused and warm to the touch.
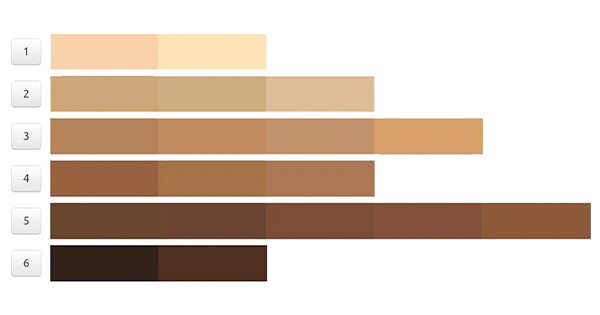
The assessment identified a circumferential lower limb wound with a wound bed displaying a combination of slough, friable granulation tissue and there was an accompanying purple rash/discolouration to his skin (Figure 1).
The wound was extremely painful, and his pain score was 9 (visual analogue scale 1–10). He informed the practice nurse that the wound appeared suddenly and that he had no previous history of ulcerations or underlying conditions pertaining to his limb. The wound was negatively impacting upon his quality of life, mobility was now becoming difficult, and he was becoming increasingly dependent upon his wife and family to help with everyday activities. He was finding it very difficult to rest and sleep and was becoming increasingly anxious as the wound was deteriorating. He frequently missed meals as he stated the wound pain often left him with no appetite and so had seen a recent loss in weight.