Nurses play a central role in delivering culturally competent care and addressing health inequalities. As frontline professionals, they are uniquely placed to identify gaps in clinical practice, such as the historical bias of assessment tools towards light skin tones and advocate for inclusive solutions. The nursing leadership in Wales has collaborated with partners to embed skin tone-inclusive protocols into clinical practice,
update education programmes and revise national guidelines.
This article explores how the nursing and midwifery community in Wales is advancing equitable care through standardised digital documentation, inclusive assessment tools, and a nationally coordinated approach. By integrating skin tone into clinical assessments, Wales is setting a precedent for anti-racist healthcare, ensuring that all patients receive safe, dignified and equitable care.
Recognition of skin tone diversity is an essential yet often overlooked aspect of wound care (Dhoonmoon, 2025). Diagnostic accuracy relies on clinicians’ ability to identify visual cues such as erythema, discolouration or signs of skin damage, which can present differently depending on skin tone (Dhoonmoon, 2025). When diagnostic frameworks and training materials are predominantly designed around light skin tones, challenges in recognising and responding to clinical signs across diverse skin presentations may arise. This can contribute to variability in care delivery and impact patient safety outcomes (Gunowa et al, 2021). In leg ulceration, timely and accurate assessment is crucial because prevention and treatment depend on clinicians’ ability to correctly evaluate skin changes (Mukwende et al, 2020).
Leg ulceration affects a significant proportion of the United Kingdom (UK) population. A population-based study of 3,000 people estimated that 2% of adults experienced a lower limb ulcer between 2017 and 2018, equivalent to approximately 1 million cases (Guest et al, 2020). Crucially, evidence shows that approximately 80% of chronic wounds can heal with timely and appropriate intervention (Guest et al, 2020).
Inaccuracies at the diagnostic stage can delay healing, increase recurrence and raise costs to the NHS. For patients with dark skin tones, under-recognition of early signs intensifies these risks, undermining the national commitment to equitable care (Gunowa et al, 2021). Addressing potential disparities through educating healthcare staff is essential for enhancing healthcare equity and improving outcomes across diverse populations (Cole and Waller, 2023).
Equity, diversity, and inclusion (EDI) are embedded within the Welsh Government’s strategic commitments to health and social care, as outlined in frameworks such as the Strategic Equality and Human Rights Plan (2025–2029) and the Anti-Racist Wales Action Plan. Translating these principles into wound care requires more than awareness: it demands structural reform and cultural transformation across clinical practice, education and service delivery.
In Wales, the integration of EDI into wound care has historically been driven by collaborative and voluntary efforts rather than statutory mandates. Nonetheless, progress has been achieved through the co-development of educational resources, clinical tools and service models that reflect the diversity of skin tones and lived experiences.
Rather than following external models, Wales offers its own valuable and transferable insights into embedding equity within clinical care, grounded in a rights-based approach, inclusive policy design and a commitment to reducing health inequalities across all communities.
This paper reports examples from Wales illustrating how challenges in leg ulcer management can catalyse innovation, presenting practical recommendations for inclusive, evidence-based and patient-centred approaches across the UK.
How skin tone influences the recognition, progression and healing of leg ulcers
Leg ulceration is a common and costly condition, driven largely by chronic venous insufficiency, lymphatic disease, arterial compromise or a combination of these factors (Raffetto et al, 2021). The underlying pathophysiology often presents first as subtle skin changes such as erythema, oedema, warmth or early breakdown of fragile tissue (Dhoonmoon, 2025). For patients with light skin tones, redness is frequently the first sign clinicians recognise. However, in patients with dark skin tones these cues may appear differently, erythema may be masked, pigmentation changes can be more difficult to identify; signs such as induration, pain or heat may be more reliable (Black and Simende, 2020). Without awareness of these variations, the earliest stages of deterioration may go
unnoticed.
Delayed recognition can allow venous hypertension or pressure damage to progress unchecked, leading to larger, more complex ulcers that are slower to heal and at higher risk of infection (Labropoulos, 2019). This increases treatment costs through more intensive dressing regimens, longer use of compression therapy and greater reliance on community nursing services (Campbell and Carradice, 2024). For patients themselves, the impact is profound with extended pain, loss of mobility, social isolation and reduced quality of life. Missed or late diagnoses in patients with dark skin tones are not only a matter of inequity, but also of avoidable harm. Recognising the challenges and inconsistencies in clinical practice, the All Wales Tissue Viability Nurse Forum (AWTVNF) developed the Standards for Leg Ulcer Care in Wales (AWTVNF, 2024). Endorsed by the CNO for Wales, these standards aim to promote equitable, evidence-based care for individuals across the Welsh population. Initiatives such as ‘Mind the Gap’ (Mukwende et al, 2020) have drawn attention to how clinical education materials often default to white skin, overlooking how conditions present in Black and minority ethnic populations. Gunowa et al (2021) and other expert recommendations (Wounds UK, 2021) have highlighted that educational gaps translate directly into practice variation and unequal outcomes. Despite this, research into wound care in diverse populations remains limited, leaving clinicians without robust evidence to guide practice.
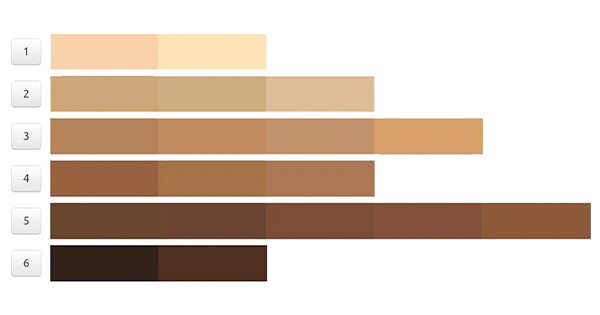
The Skin Tone Tool [Figure 1] is designed to support clinicians in recognising early skin changes across a spectrum of skin tones (Dhoonmoon, 2025). The tool offers a simple, validated and cost-effective solution. Based on a graded visual scale matched to the inner arm, it has already been implemented in contexts such as skin cancer risk screening and sun protection guidance. By providing a more objective alternative to binary skin classifications, it supports more equitable diagnostic practices in wound care (Wounds UK, 2021).
By presenting standardised visual cues, it reduces reliance on subjective interpretation and complements established assessment frameworks such as the PURPOSE-T risk tool (Fletcher, 2023). Used in conjunction with structured wound assessment charts and care pathways, the tool helps to ensure that signs of deterioration are not overlooked (Wounds UK, 2021). It also provides a common language for staff education, enabling teams to train consistently and inclusively. As leg ulceration continues to place a burden on health services, embedding skin tone tools into everyday assessment offers a practical step toward equity, safety and improved outcomes for all patients.
What challenges emerged in implementing the Skin Tone Tool in Wales?
With a population of just over 3.3 million (Office for National Statistics [ONS], 2025), Wales offers a unique opportunity to pilot national healthcare initiatives. Its size allows for flexible implementation, while its demographic and clinical diversity mirrors challenges seen across the wider UK. The structure of NHS Wales, (comprising seven health boards, three NHS trusts and several special health authorities) supports a ‘Once for Wales’ approach, enabling standards to be developed collaboratively and applied consistently across the system (NHS Wales, 2022). According to the 2021 census, approximately 90.6% of the Welsh population identify as ‘White’, 2.9% as ‘Asian, Asian Welsh or Asian British’ and 1.6% as ‘Mixed or Multiple Ethnic Groups’, reflecting an increase in ethnic diversity since 2011 (Welsh Government, 2022). Policy drivers in Wales have also been influential. The ‘Anti-Racist Wales Action Plan’, launched in 2022 and updated in 2024, set out a clear expectation that health services must address inequities and provide inclusive care (Welsh Government, 2024a). For nursing and midwifery, this emphasis is reinforced by the CNO Strategic Vision 2025-2030, which strengthens equity and diversity at the centre of professional leadership. Around 40% of the NHS workforce in Wales are nurses and midwives, with an increasing proportion from black and minority ethnic backgrounds, currently around 14% and growing (ONS, 2025). Taken together, these data highlight the importance of culturally competent practices and equitable diagnostic approaches to ensure consistent care for all (Welsh Government, 2024b).
This demographic shift highlights that equity must extend beyond patient care: it should also involve fostering an inclusive professional culture where healthcare staff feel equipped, supported and valued. Within wound care, skin tone recognition has emerged as a practical and visible means of advancing these commitments. The urgency of this work was amplified during the coronavirus disease (COVID)-19 pandemic, which highlighted significant disparities in health outcomes among minority ethnic communities.
Due to their prevalence among patients with complex, chronic disease(s), lower limb wounds, particularly leg ulceration, place a substantial burden on the NHS. In England alone an estimated 739,000 cases were reported in 2019, with associated healthcare costs of £3.1 billion (National Wound Care Strategy Programme, 2023). Inequities in clinical recognition especially across diverse skin tones can exacerbate these challenges, leading to delayed or suboptimal care. Wales demonstrates how embedding tools such as a skin tone resource into wound assessment can operationalise equity. Through strategic alignment of digital innovation, policy support and collaborative practice, equity can be assured within wound care services.
How was the skin tone assessment digitally integrated into Welsh wound care?
One of the most distinctive features of the Welsh approach to equity in wound care has been the use of digitalisation to drive consistency. The development of the Welsh Nursing Care Record (WNCR) is central to this agenda. Launched as a national nursing inpatient record for acute care, the WNCR replaces local variation with a single digital platform (Digital Health and Care Wales, 2025). Designed through extensive consultation with expert groups, including the AWTVNF and Wales Wide Digital Nurse leaders, it provides an opportunity to ensure that core elements of wound care are embedded from the outset.
In October 2023, skin tone considerations were formally embedded into the pressure damage assessment tool within the WNCR. Although the Welsh Government did not mandate this change, health boards and trust were empowered to implement it based on local readiness and capacity. This flexible approach aligns with Wales’ enabling policy ethos, which prioritises professional judgement and contextual responsiveness over prescriptive directives.
Adoption has varied across health boards, but the expectation remains clear: skin tone assessment should become a routine part of clinical practice. This expectation is grounded in evidence-based guidance and professional consensus, recognising the importance of equitable care in pressure damage prevention and assessment. The WNCR prompts clinicians to consider and document early skin changes across diverse patient groups. In areas where the digital record has not yet been fully adopted, paper-based wound assessment charts have been updated as a temporary measure, ensuring that progress is not stalled.
By standardising pressure damage and repositioning assessments across Wales, the WNCR generates consistent data that can be used to monitor outcomes and identify inequities. This creates a feedback loop in which evidence can inform practice and practice can refine policy.
Digitalisation is not just an administrative upgrade, it is a tool for cultural change. By embedding equity into the daily workflows of clinicians, Wales is making inclusivity routine practice rather than exception.
Overcoming barriers: Strategies for equitable skin tone assessment in Wales
The integration of skin tone recognition into leg ulcer care in Wales has surfaced important learning opportunities. Implementation has varied across health boards due to differences in IT infrastructure, staff training timelines and governance processes; this variation reflects the realities of adapting new practice within complex systems. Importantly, the WNCR is now live across all inpatient areas, providing a consistent foundation for further development.
Early adopter sites have demonstrated how inclusive pressure ulcer care can be successfully embedded into routine practice. Their experiences offer valuable insights into overcoming resource constraints, streamlining training and improving documentation. These sites have shown that when clinicians are supported with clear tools and evidence-based guidance, they are more likely to embrace new approaches and move beyond traditional observation methods, particularly in assessing subtle skin changes in individuals with dark skin tones.
Across Wales, the AWTVNF continues to champion inclusive documentation and practice. Their work is helping to build momentum, foster peer learning and ensure that skin tone assessment becomes a standard part of equitable pressure ucler care. See Figure 3 to view the participating Health Boards across Wales.
In Wales, the relatively small ethnic minority population presents challenges in gathering a wide range of lived experiences from patients with dark skin tones. This can limit the availability of robust patient-reported outcomes, which are essential for shaping equity initiatives through genuine collaboration. To ensure these efforts are truly inclusive, it is important to balance professional insight with direct patient engagement.
Support for internationally educated nurses has been a positive step toward diversifying the workforce. However, it is equally important to amplify the voices of second- and third-generation minority ethnic communities within Wales, whose experiences may differ and whose perspectives are vital in shaping culturally responsive care. Learning from early engagement and community partnerships can help ensure that equity work reflects the full spectrum of Wales’ population (Rajpoot et al, 2024).
Despite these challenges, meaningful solutions remain within reach. Even small-scale staff and patient surveys can highlight inequities and guide targeted improvements. Undergraduate nurses offer valuable perspectives, particularly as they engage with inclusive resources, such as the Skin Tone Tool, during their training (Wounds UK, 2021). Integrating this tool into care pathways, electronic health records and educational programmes not only enhances immediate clinical practice but also embeds equity as a foundational standard for future generations.
Incorporating cultural awareness into continuing professional development further strengthens workforce capability, fostering confidence and competence in delivering equitable care across diverse populations (Stubbe, 2020).
Challenges persist with context-sensitive strategies, sustained collaboration across clinical, educational and governance domains and a commitment to equity. However, this collaboration of AWTVNF with the Welsh government demonstrates that inclusive leg ulcer care can evolve from an aspirational ideal into embedded, everyday practice. Progress is being made not only through policy and innovation, but also through the collective efforts of clinicians, educators, patients and system leaders who are reshaping standards of care to reflect diversity, dignity and clinical excellence.
How can clinicians apply the Skin Tone Tool in practice?
The Skin Tone Tool offers a practical resource to support more consistent and equitable assessment across diverse patient groups.
This resource can be integrated into routine leg ulcer assessments to prompt clinicians to consider how early skin changes may present differently across varying skin tones. Rather than relying solely on visible redness which may be less apparent in dark skin, clinicians are encouraged to assess additional indicators such as swelling, warmth, induration and patient-reported discomfort, which may offer more reliable diagnostic cues (Wounds UK, 2021; Dhoonmoon, 2025). The presence of a visual reference, whether in printed form or embedded within electronic health records, helps to normalise this inclusive approach and reduces the likelihood that subtle, yet clinically significant signs are missed.
Aligning the tool with updated wound assessment charts, pressure ulcer prevention protocols and the WNCR reinforces its role as a standard component of clinical workflow, rather than an optional extra [Figure 4]. Importantly, the tool is not intended to replace clinical judgement but to enhance it by offering a consistent framework supporting earlier recognition of leg ulceration across all skin tones. In doing so, it enables timely intervention, reduces delays in care and promotes safer, equitable outcomes for all patients.
Embedding equity in wound care across the UK
Lessons from these improved outcomes and the ‘Once for Wales’ approach can be applied throughout the UK. Wales has exemplified how digital innovation, cross-sector collaboration and policy alignment can embed equity into wound care practice (NHS Wales, 2022). The integration of skin tone recognition into the WNCR and the Standards for Leg Ulcer Care in Wales [see Figure 4] illustrates that systemic change is achievable at a national level (AWTVNF, 2024). The ‘Once for Wales’ approach serves as a blueprint for smaller nations seeking to standardise care, reduce disparities and support both patients and clinicians through unified protocols (Welsh Government, 2015).
Resources, such as the skin tone assessment tool depicted in Figure 1, should be viewed not as optional enhancements, but as foundational elements in the pursuit of national equity. By adopting shared standards and fostering collaboration across the UK’s health systems, the NHS can move closer to a future where no patient with a leg ulcer is disadvantaged due to their skin tone.
The integration of skin tone assessment into clinical practice has been made possible through collaborative efforts across the NHS. This work was supported by collaboration with Essity, who partnered with several NHS organisations to help integrate skin tone assessment into clinical practice. These partnerships have enabled the development and adoption of inclusive tools that support equitable care for all patients
Conclusion
Equity in wound care is central to safe, effective and compassionate patient care. Traditional assessment of leg ulceration has long relied on visual indicators such as erythema, which may not present consistently across different skin tones. This reliance introduces a risk of delayed diagnosis, suboptimal outcomes and preventable harm, particularly for patients with dark skin.
Wales has demonstrated that inclusive wound care is achievable when supported by clear policy direction, digital integration and multidisciplinary collaboration. By embedding skin tone recognition into national standards and clinical systems, Wales is leading the way in transforming equity into routine practice.
It is essential to ensure that all patients, regardless of skin tone, receive accurate diagnosis and early care. Inclusive tools and frameworks are essential to closing gaps in care and delivering enhanced clinical outcomes.
The Skin Tone Tool offers clinicians a practical way to improve accuracy and confidence in recognising early skin changes while providing a framework for educating. With updated assessment standards and integrated into digital records, it helps move equity into routine practice.
The goal now is to scale this learning across the UK. By coordinating efforts across the nations, clinicians and policymakers can collaborate to ensure that all patients receive the care they need, regardless of skin tone. This united approach will help embed inclusive practices into the heart of healthcare delivery.