The current definition of a leg ulcer is ‘a break in the skin below the knee that has not healed within 2 weeks (NICE, 2023) and is a condition that can affect large numbers of people due to a variety of reasons, such as chronic venous insufficiency (CVI), peripheral arterial disease (PAD), ageing, skin frailty and diabetes (Hogh, 2023).
In the second study of a series conducted by Guest et al (2020), it was estimated that there were approximately 1 million recorded cases of leg ulcers within the adult population of the UK during the 2017/18 study period. This represents a 36.8% increase compared to the findings of the equivalent study period conducted 5 years earlier (Guest et al, 2015).
Consequently, the associated costs of managing leg ulcers in the UK has risen to approximately £4.6 billion per annum, a substantial percentage of NHS budget and placing a huge burden on the delivery of NHS services (Guest et al, 2020). Most patients with leg ulcers are treated within the community setting (Guest et al, 2020) and a primary cost driver associated with treatment of leg ulceration is the time allocated for community nursing visits. The resource of the community nurse has been identified as comprising of up to 78% of the total expenditure associated with the treatment of leg ulceration (Guest et al, 2018; Urwin, 2022).
The Queen’s Nursing Institute (QNI, 2019) has reported a 43% reduction in community nurses over the past decade, a trend that is likely to adversely affect the delivery and quality of leg ulcer care within community services.
A similar analysis undertaken within Wales detected a comparable burden in terms of prevalence and cost of chronic wounds generally, calculating 6% of the Welsh population experience chronic wounds costing approximately 5.5% of annual NHS Wales expenditure (Phillips et al, 2015). A follow-up study looking specifically at the costs associated with venous leg ulcers (VLUs) suggested this wound type alone represents 1.2% of the annual NHS Wales budget with direct costs to manage a patient with a VLU averaging £7,706 per patient per annum (Phillips et al, 2020).
While the evidence presented of steeply rising prevalence rates for leg ulcers and huge costs to health services is highly important, the impact on the individual living with a leg ulcer is enormous. Research has repeatedly highlighted the increased morbidity and poor health-related quality of life associated with leg ulceration, from the effects of pain, high levels of exudate and offensive odour to the increased rates of depression, anxiety and social isolation (Green et al, 2014; Smith et al, 2023). When taken with consideration to another finding of the Guest et al paper (2020) that less than half of the VLUs identified healed within the study year (37%), effectively leaving over 600,000 individuals still living with an unhealed leg ulcer after 12 months, the need for change and improved practice was clear and indisputable.
Impact of delayed diagnosis and variations in care
Several factors have been proposed to explain the rising burden of leg ulcers on individuals and services in the UK. These include sub-optimal wound management, stemming from a lack of evidence-based practice, inadequate diagnosis and assessment, variations in care and a lack of education and training for healthcare professionals (Guest et al, 2020; Phillips et al, 2020).
Patients with leg ulceration are often left undiagnosed with regards to the underlying aetiology of their ulcer, leading to inappropriate treatment, particularly regarding compression therapy (Guest et al, 2020). Compression therapy has long been considered the gold standard treatment for patients with a venous component to their ulcer aetiology (Meara et al, 2012), yet if there is a lack of diagnosis as to whether the ulcer is of venous, arterial, mixed or atypical in origin, it is difficult to instigate the correct compression therapy when indicated, or indeed make an onward referral for further multidisciplinary input.
Furthermore, failure to identify the aetiology of the ulcer often leads to patients being sub-optimally managed for many months with increasing risk of delayed wound healing and development of wound complications (Wounds UK, 2019). Recent observations by the Legs Matter campaign highlighted the detrimental effects on patient health when there is a delay in assessment and the use of inappropriate therapy for leg-related conditions. The campaign highlights the critical importance of timely intervention, as failure to promptly address this requirement can lead to significant patient harm.
Lack of time and resource are often blamed for inadequate or delayed assessment of patients with leg ulcers, alongside poor access to specialist services and lack of sufficient training to perform supportive examinations, such as a Doppler test, to exclude the presence of significant arterial disease and support a diagnosis of venous or mixed disease leg ulceration (Wounds UK, 2019). This is again supported by the findings of both Guest papers where it was identified that only 15% of records for patients with lower limb ulceration had a recorded Ankle Brachial Pressure Index (ABPI), and 25% of patients with a wound had an undiagnosed aetiology, 9% of which was related specifically to leg ulceration (Guest et al., 2020). A Cochrane review comparing no compression versus compression therapy for treating VLU concluded that the use of compression therapy is likely to heal ulcers more quickly, increase the number of patients healed within 12 months, reduce pain and improve some aspects of quality of life (Shi et al, 2021). A recent update to a previous Cochrane review also confirmed that continued compression therapy after healing reduces ulcer recurrence within 6 months (De Moraes Silva et al, 2024). While it is understood that delivering efficient and effective healthcare services can be challenging in current times, it must not become the accepted norm to repeatedly deny patients access to evidence-based treatment because leg ulcers are not seen as high priority compared to other conditions or tasks. Patient-centred care must be at the heart of every service delivering care to patients with wounds and recognition given that early assessment and optimised treatment are key to positive patient outcomes, reduced time to healing and thus less demand on time and resource in the long-term.
Alongside variations with assessment, diagnosis and intervention processes, it is also important to recognise the impact of other variations in care with regards to leg ulcer practice. Patients with chronic wounds are cared for in a variety of settings across primary, community and secondary care where there can be varying levels of expertise and poor understanding of where and when to seek specialist advice due to a lack of clear referral and treatment pathways (Guest et al, 2018). The patient experience is consequently poor with a lack of transparent communication between services and no ownership and accountability by clinicians for their care (Squitieri et al, 2020). Unwarranted variations lead to poorer outcomes, extended healing times, increase in overall costs and clinician time and increased suffering for the individual living with leg ulceration (Guest et al, 2015; Adderley et al, 2017).
Within Wales, an All-Wales collaborative approach to practice and policy is advocated by the AWTVNF who have raised awareness and the profile of wound care across all levels of service provision and published guidelines for practice across several pertinent areas of the speciality. Despite this work, however, there are still variations seen across the Health Boards within Wales which include the types of specialist wound services on offer, how they are accessed and the processes of care that are followed (Mahoney and Simmonds, 2020). All-Wales guidance is available and utilised with regards to pressure ulceration, for example, but not necessarily for all conditions sitting under the tissue viability umbrella, including previously leg ulceration.
National Recommendations
Following debate in the UK Parliament House of Lords regarding concerns highlighted by the Burden of Wounds Study (Guest et al., 2015), the National Wound Care Strategy Programme (NWCSP) was launched by NHS England and NHS Improvement in late 2018. The aims of the NWCSP were multiple, encompassing improving the quality of care being delivered to people with leg and foot ulcers, pressure ulcers and surgical wounds through promotion of evidence-based practice and reduction of unwarranted variation in care for an individualised wound through to national service level (NHS England, 2018).
As part of their lower-limb working stream, the NWCSP produced a set of recommendations for leg ulcers to provide clear advice about the fundamental evidence-based care that should be provided for people with leg ulcers to improve outcomes and make more effective use of healthcare resources (NWCSP, 2023). The recommendations outline a pathway of care from early assessment and diagnosis through to management of healed ulceration, including advice on onward referrals and when to escalate treatment.
One of the most defining elements of this guidance was the recommendation for immediate and necessary care for leg ulcers which challenged the established thinking around safe implementation of compression therapy. Historically, compression therapy was only instigated following a full vascular assessment of the patient to exclude the presence of PAD, and typically included a Doppler test to measure ABPI. Until an ABPI was available to form part of the assessment, it was considered unsafe to commence compression in case PAD was present and harmful side effects were incurred (Scottish Intercollegiate Guidelines Network [SIGN], 2010).
Alongside an inexperienced and under-trained workforce within leg ulcer management, this historical position has created fear among nurses that compression is a high-risk and complex therapy which should only be applied with caution (Field, 2004; Pernissi et al, 2023). A perceived culture of blame within nursing and the potential for legal repercussions may also contribute to fear and the choice to ‘err on the side of caution’ when instigating compression (Ritchie et al, 2018). While it is of course important to assess the patient to ensure compression is applied safely and practitioners are trained on application techniques, there needs to be a move away from the perception of it being potentially ‘dangerous’ towards an understanding of the key concepts of compression therapy and the benefits it provides to develop confidence with its initiation and application. Once significant PAD has been ruled out, compression therapy is a safe and effective treatment option. It is also important to recognise that an ABPI measurement should only form part of diagnostic decision-making around leg ulcer aetiology and suitability for compression alongside patient history, presence of risk factors and clinical signs and symptoms (BLS, 2018). These should offer a large part of the information needed to support diagnosis, with ABPI offering supplementary information — again, there needs to be a move away from over-reliance on ABPI as the single most important assessment criterion for starting compression therapy.
The vital need for early instigation of compression on first presentation of a patient with a leg ulcer even when time or resource constraints mean a full vascular assessment cannot be performed was recognised by the NWSCP (2023) and led to the following recommendation: ‘Those without red flag symptoms and at low risk of pressure damage over bony prominences should be offered first line mild graduated compression (20mmHg or less at the ankle)’ until a comprehensive assessment is performed within 14 days. The recommendation for wounds on the leg to be treated with mild compression is based on the British Lymphology Society view that, providing people with ‘red flag’ symptoms are excluded, the benefits of first line mild compression outweigh the risks, even for people without obvious signs of venous insufficiency (BLS, 2018).
Due to there being a devolved government within Wales, NHS services are delivered under the umbrella of NHS Wales as opposed to NHS England. While definite learnings are taken from guidance issued both within the UK and internationally, the NWCSP in essence was an NHS England initiative involving stakeholders and clinicians within England predominantly. There is considerable crossover in wound care practice between both Wales and England, but there is also the potential for there to be local differences in services and set-up due to working under different government directives and budgets. Within Wales there is a growing importance being placed on delivery of safe, timely, effective, efficient, equitable and person-centred health services evidenced within the ‘A Healthier Wales’ strategy (Welsh Government, 2018), and a value-based healthcare (VBHC) approach is being adopted nationally. Key areas of focus for embedding VBHC within healthcare pathways across NHS Wales include Prevention, Early Accurate Diagnosis, Optimising Interventions and Supportive Treatments (Welsh Value in Health Centre, 2021), which align perfectly with the approach required to improve the quality and value of wound care services and leg ulcer management in Wales. As such, it was decided to develop a set of standards for leg ulcer care that were specific to the Welsh population that were recently launched by the AWTVNF in May 2024 (AWTVNF, 2024).
Standards for Leg Ulcer Care in Wales
The standards were developed to define the minimum standard of care that should be delivered for LU prevention and management, promoting consistent clinical practice and prompt assessment and intervention to optimise outcomes and healing rates for people with LU in Wales (AWTVNF, 2024). The standards recognise the need for effective, early intervention in the form of immediate, first-line reduced compression therapy in the absence of significant arterial risk factors, red flags or contraindications.
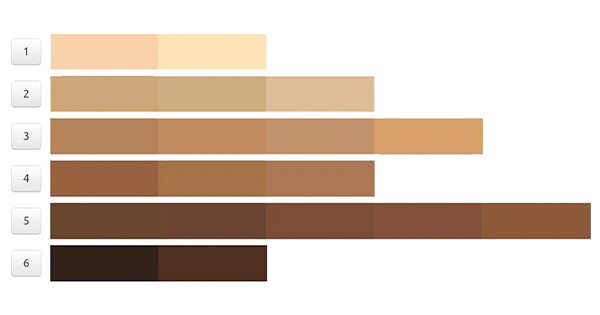
On first presentation of a patient with an untreated leg wound, it is recommended that an initial contact assessment form is completed to include ulcer history, wound and skin tone assessment and determination of patient goals, needs and capabilities. Assessment for risk factors, red flags and cautions should then take place [Box 1] to determine the next steps for compression management – in the absence of risk factors and red flags, reduced multicomponent compression bandaging delivering up to 20mmHg, or Class 1 hosiery should be applied.
What is mild or reduced compression?
The World Union of Wound Healing Societies (2008) defined compression levels using the following terms:
- Mild (less than 20mmHg)
- Moderate (20–40mmHg)
- Strong (40–60mmHg)
- Very strong (greater than 60mmHg).
Mild compression is indicated for a range of lower-limb wounds, such as skin tears, as well as for immediate and necessary care on initial presentation with leg ulceration. Mixed arterial-venous disease ulcers are recommended to be treated with mild to moderate compression which has been shown to increase venous return, reduce oedema and increase arterial perfusion (Mosti et al, 2012; Vowden et al, 2020).
Mild compression can be administered with some types of compression bandaging and hosiery. British standard Class 1 hosiery would be the option for immediate and necessary care as it is the only class which delivers ≤20mmHg at 14-17mmHg (Wounds UK, 2021), with RAL Class 1 delivering slightly over the recommendation at 18-21mmHg). Only some types of compression bandaging could be considered viable options as with the multiple factors that can affect sub-bandage pressure, such as bandage width, extension and overlap, it can be difficult to control application at a reduced level which could affect confidence that no more than the recommended 20mmHg is being applied.
Some bandage manufacturers do not stipulate a pressure applied by the bandage in mmHg or discuss the indications for use only in terms of within certain ABPI levels e.g. >0.5 or >0.8 — this can make it difficult to interpret if usage is thus permitted within the criteria stipulated in the published guidance.
The Standards for Leg Ulcer Care in Wales document (AWTVN, 2024) advises that a Class 1 hosiery or garment is indicated where there is a normal leg shape and where exudate is easily contained within a dressing, with compression bandaging being the recommended choice where leg shape is unsuitable for hosiery and exudate is at a level that it is not easily contained within a dressing. Patient preference should also be considered and discussed as part of the assessment process.
Optimum treatment for VLU is the application of strong compression, i.e. >40mmHg, to heal these wounds as quickly as possible (Vowden et al, 2020), and this is very much the recommendation from both the NWCSP recommendations and the Standards for Wales. While mild compression is the safest and quickest way to instigate compression prior to full vascular assessment, the aim should always be to increase compression to a therapeutic strong level as soon as possible for those people where a pure venous aetiology to their ulceration has been established. This should be within 14 days of presentation to minimise the impact of implementing a sub-optimal dosage of compression longer-term where strong compression is indicated (AWTVNF, 2024; NWSCP, 2023).
UrgoKTwo Reduced
UrgoKTwo Reduced is a 2-layer multi-component compression system consisting of an inelastic and elastic bandage. UrgoKTwo Reduced has been specifically developed to deliver a reduced level of compression (around 20mmHg at the ankle), in line with the national recommendations for immediate and necessary care and for patients with mixed aetiology ulcers.
The first layer, KTech, is an inelastic bandage consisting of viscose and polyester wadding with a knitted polyamide and elastane layer that has multiple functions. The short-stretch nature of the bandage provides a higher working pressure and lower resting pressure to improve venous return and reduce oedema, while distributing pressure uniformly over the surface of the leg. The layer also provides protection and absorbency.
The second layer, KPress, is an elastic cohesive bandage made from acrylic, polyamide and elastane. KPress provides the additional compression necessary to achieve the required therapeutic pressure of 20mmHg while maintaining recommended resting pressures necessary to maintain improved blood flow. The conformity of the elastic bandage also reduces the potential for bandage slippage as oedema decreases following application (Junger et al, 2009; Lantis et al, 2020).
The combination of the two layers means that UrgoKTwo Reduced provides the dynamic static stiffness profile to treat venous insufficiency, and tolerable resting pressures to promote patient comfort both day and night (Benigni et al, 2007). This can encourage patient engagement with compression therapy, and thus improved outcomes (Dowsett, 2022; Lantis et al, 2020). The bandage design enables it to stay in place for up to 7 days and trials have indicated that therapeutic pressures are maintained consistently over that time period (Junger et al, 2009).
Unique to the UrgoKTwo/UrgoKTwo Reduced compression systems are the pressure indicators printed on each bandage. These guide the clinician applying the bandage to ensure the correct stretch and overlap of each bandage is applied consistently and accurately to deliver the correct therapeutic pressure level. This can help support the clinician with confident application of compression therapy, overcoming some of the fears associated with applying bandages too tightly and over-compressing limbs, thus promoting usage for all patients where clinically indicated (Dowsett, 2022).
The pressure indicators can also support confidence that compression bandaging is being safely applied for immediate and necessary care within the parameters recommended by the NWCSP and Standards for Leg Ulcer Care in Wales for patients where compression bandaging is the best option — for example, applying ≤20mmHg where there is abnormal limb shape and higher levels of exudate. This may not be the case for all compression bandages offering a reduced option, or where high compression systems must be modified to try and reduce sub-bandage pressures.
Several publications have supported the integration of the UrgoKTwo systems into clinical pathways of care, achieving improved healing rates and timely and consistent care (Milne and Jones, 2018; Dowsett, 2022; Phillips et al, 2023). One of the key attributes of choosing UrgoKTwo and UrgoKTwo Reduced for first line use in these clinical evaluations was its ease of use, enabling continuity of care across different settings, and the robust evidence to support efficacy. It is also well-tolerated and accepted by patients (Dowsett, 2022; Stucker et al, 2021)
Conclusion
Leg ulcers place a huge, but largely unnecessary burden on NHS services, costs and patients. Delayed diagnosis and variations in care need to be overcome to reduce this burden, alongside improved education and support for all levels of healthcare professional.
National guidelines produced by the NWCSP and more recently the Standards for Leg Ulcer Care in Wales (AWTVNF, 2024) have recommended steps to provide immediate and necessary care to all patients presenting with leg ulceration to prevent delays in instigating compression treatment and to optimise healing outcomes.
UrgoKTwo Reduced offers an easy-to use and effective option for providing first line 20mmHg of compression prior to full vascular assessment and in the absence of red flags, promoting confidence in clinicians that they are providing continuous, consistent, and comfortable compression to their patients.