Wound dressing performance is an important component of wound care delivery. A vast selection of advanced wound dressings are aimed at providing the ideal conditions to advance healing for patients with chronic wounds (NICE, 2016). Knowledge of how wound dressings properties can aid wound healing is critical for ensuring health professionals select the right product for patient safety and clinical effectiveness, whereas inappropriate dressing choice can limit wound healing (Rippon et al, 2012) and increase financial expenditure. In England, prescription costs for advanced wound and antimicrobial dressings in primary care alone are over £100 million per year, with £20 million estimated as being spent on silver-containing dressings (NICE, 2016).
Wound care knowledge
Chronic wound care in the community is usually undertaken by nursing teams with varying degrees of education and training, which greatly influences wound care practice (Gray et al, 2018). Tasks such as wound dressing selection and changes are common clinical duties for nurses working in the community setting but a limited understanding of dressing wear time can lead to an increased frequency of dressing changes. This is evidenced by a study that found wound inspection was the main driving force for foam dressing changes in patients with acute wounds, rather than clinical need or assessment (Blackburn et al, 2018). Therefore, increasing education and skills in wound management could help support confidence in decision making and improve quality of care.
Wound dressing selection should involve a multifaceted holistic approach, with a full clinical assessment of an individual’s wound status, needs and preferences before selecting the most appropriate wound dressing for each patient, with a particular focus on dressing change (NICE, 2016). However, research has shown that many healthcare professionals do not feel confident in making these decisions, with a tendency to rely on senior colleagues for support, or engage in ritualistic practices such as frequent dressing changes due to a perceived need to inspect the wound for signs of healing (Blackburn et al, 2019). This means that the performance of many wound dressings are not optimised, leading to increased costs, delayed wound healing and trauma and distress to the patient (Brindle and Farmer, 2019). Decisions about dressing choice and dressing changes are further complicated by a lack of robust high-quality clinical evidence to support the use of advanced and antimicrobial wound dressings for the management of chronic wounds (NICE, 2016). Reducing the number of available products to healthcare professionals and encouraging them to use a holistic approach to wound management has been highlighted as essential for managing the real world cost of wound care (Blackburn and Ousey, 2022). Important aspects of the holistic approach include extending dressing wear time and minimising the number of dressing changes (wound dependent), but the evidence suggests that many healthcare professionals need further support in the form of training and education if they are to feel confident to change their practice and trust their clinical judgement.
Aims/objectives
Our study aimed (i) to investigate the effects of an educational programme and dressing-specific education alongside the introduction of Mepilex Border Comfort dressings on nurses’ frequency of dressing changes in the home care setting (ii) to qualitatively explore the impact of education on nurses’ clinical practice, decision making and confidence.
Methodology
There were three district nursing teams within the Manchester University National Health Service (NHS) Foundation Trust area involved over a four-week period, participants were clinical staff working within one of the district nursing teams. The teams were considered comparable in terms of size, patient population and staffing. Allocation to three study groups was undertaken locally by the principal investigator through random selection of each site to one of the following teams:
Standard care
Dressing-specific education
General and dressing-specific education group.
Standard care group (control group): participants were instructed to follow standard practice for all new wounds considered as being appropriate for management with bordered foam dressings.
Dressing-specific education group: participants received wound dressing-specific education delivered by a representative of the manufacturer at each site (lasting approximately 20–60 minutes) before being instructed to apply Mepilex Border Comfort to all new wounds considered as appropriate for management with bordered foam dressings.
General and dressing-specific education group: participants received the wound dressing-specific education and in addition completed an online general wound care training education programme (Challenges in Wound Care), developed by the University of Huddersfield. Participants were required to apply Mepilex Border Comfort to any new wounds considered appropriate for management with bordered foam dressings.
Participants completed a participant information file (PIF) collecting information about age, gender, job role/grade, years of experience and previous wound care/dressing education and completed a dressing change log at each visit for each patient.
Qualitative interviews
Semi-structured virtual interviews were conducted during January–March 2022 with five participants from each of the two education groups who were identified through purposeful sampling — used in qualitative research for the identification and selection of information-rich cases for the most effective use of limited resources. The interviews explored the impact of education on nurses’ clinical practice, decision making and confidence.
Ethical approval
Health Research Authority (HRA) ethical approval was granted by Health and Care Research Wales (HCRW). Research governance approval was received from the NHS Trust and School Research and Ethical Approval was received from the University of Huddersfield (SREIC/2021/020) for the interviews.
Educational intervention
There were 16 wound dressing logs received from the standard care group, with 8 patients represented, 8 wound dressing logs were received from the dressing-specific education group, with 3 patients represented and 6 wound dressing logs were received from the general and dressing-specific education group, with 3 patients represented. Information reported included: patient identifier; date of dressing; reason for dressing change; dressing type; wound area; days since previous dressing change and whether the change was considered necessary. The main outcome for the study was taken as the duration between consecutive dressings. However, only the standard care group completed the participant information file, the other groups failed to do so.
Results
Standard care group
A summary of the information provided in the dressing logs of the standard care group (control group) is provided in Table 1.
Treatment of 3 patients in the standard care group was recorded on multiple occasions. Treatment of 5 patients was each recorded on a single occasion. The most commonly used dressing was Kliniderm Silicone Border; used at 10 of the 16 reported wound dressing changes. Mepilex Border Comfort was used at four wound dressing changes; with Allevyn Life and Tegaderm Adhesive both used on one occasion each. There was a large variation in wound sizes, with wounds from 375cm2 to ‘pin-size’ being treated. The average frequency of wound dressing change at this site was 4.69 days (standard deviation [SD]: 2.36 days). The average frequency per patient was 4.71 days (SD: 1.69 days). Of the 14 wound treatment episodes for which a reason for dressing change was recorded, four (28.6%) were exclusively due to a planned dressing change being scheduled (i.e. no unanticipated problems with the wound and/or dressing). Issues including leakage, dressing falling off or creased or strikethrough/visible exudate were reported in 10 wound dressing episodes (71.4%).
Participants who reported their roles included: three district nurses, four community staff nurses, two senior nursing assistants and one healthcare support worker; with salary bands from three to seven inclusive represented. Participants had an average age of 41.6 years (SD: 8.67 years; age range: 28 to 53 years), with an average of 9.33 years of experience (SD: 4.42 years; experience range from 4 to 16 years). All had received some form of education in wound dressing; many reported multiple modes of education including: online; given by company representatives; in-house; informal training from colleagues; study days; and attendance at wound management modules delivered by a local higher education provider.
Dressing-specific education group
A summary of the information provided in the dressing logs of the dressing-specific education group is provided in Table 2.
The treatment of 2 patients in the dressing-specific education group was recorded on multiple occasions; with the treatment of one patient recorded on a single occasion. Mepilex Border Comfort was used at all wound dressing changes. There was variation in wound sizes but, where reported, were generally smaller than those reported in the standard care group, with no wounds reported to have an area in excess of 15.75cm2. The average frequency of wound dressing change at this site was 2.38 days (SD: 1.73 days). The average frequency per patient was 2.17 days (SD: 1.03 days). There were 2 dressing changes in this group were conducted even though they were not considered necessary.
Of the 8 wound treatment episodes for which a reason for dressing change was recorded, five (62.5%) were exclusively due to either a planned dressing change being scheduled or an initial patient assessment (i.e. no unanticipated problems with the wound and/or dressing). Issues including dressing falling off or strikethrough/visible exudate were reported in the remaining three wound dressing episodes (37.5%).
A summary of the information provided in the dressing logs of the general and dressing-specific education group is provided in Table 3.
Treatment of 2 patients in this group was recorded on multiple occasions; with the treatment of one patient recorded on a single occasion. Mepilex Border Comfort was used at all wound dressing changes. There was variation in wound sizes, but where reported, were generally smaller than those reported in the standard care group, with no wounds reported to have an area greater than 7cm2 and about the same size as wounds reported in the dressing-specific education group. The average frequency of wound dressing change at this site was 5.33 days (SD: 2.05 days). The average frequency per patient was 6.00 days (SD: 2.00 days). Of the 5 wound treatment episodes for which a reason for dressing change was recorded, three (60.0%) were due to either a planned dressing change being scheduled or an initial patient assessment (i.e. no unanticipated problems with the wound and/or dressing). Strikethrough/visible exudate was reported in the remaining two wound dressing episodes (40.0%).
Comparison of site results
Insufficient data were collected from all groups, in particular both education groups, to assess the group effect via statistical testing, or to derive meaningful confidence intervals around effects. Furthermore, there were some differences in the size of wounds treated across the three groups, which could potentially contaminate inferences relating to wear time. Although the dressing-specific education and general and dressing-specific education groups featured exclusively the Mepilex Border Comfort wound dressing, this dressing was also used for the treatment of certain wounds in the standard care group. This commonality may potentially reduce the expected difference in wound-related outcomes.
Due to the low sample size and group imbalances, the analysis conducted on the data was limited to descriptive procedures without inferential testing. There is insufficient evidence to conclude that either the education package with or without additional training results in better outcomes. However, some differences in the days between successive dressing changes in each group were recorded and are summarised graphically in Figure 1.
Interview data analysis
Interviews with 10 participants (5 from each education group) were conducted via telephone or Microsoft Teams, were audio recorded and lasted between 25–50 minutes. Participants were provided with information sheets and completed consent forms before the interview and were informed that they had the right to withdraw at any time up to the point of interview analysis.
Interview recordings were transferred to an encrypted storage device and identified with a code, transcribed verbatim and then the audio recordings were destroyed. Transcripts were anonymised to remove any information that might have identified the respondents and entered into NVIVO qualitative data analysis software (QSR International) to aid data management analysis and retrieval. Thematic analysis was used to identify patterns and common themes among the participants’ experiences, revealing four main themes and 8 sub-themes (Table 4).
Theme 1: wound care education
Previous wound care education was limited and consisted of informal and formal education.
Informal education: learning from others
Knowledge was often obtained through experience and informal training was delivered ‘on the job’ by senior colleagues. There was a tendency to ‘do something because someone else is doing it’.
‘I don’t think we get formal training. I think a lot of it is you have to learn as you go and if you’ve not got a good teacher, you’ve just got to kind of get on with it… I think probably we don’t get enough training on wound care.’ District Nurse Sister, specific education group
Formal education
University courses provided some structured education on wound care and wound dressings.
‘I think at uni we literally did a day… But then through my Trust I did training for compression and managing leg ulcers.’ Community Staff Nurse, general and specific education group
Ad hoc study days and manufacturers delivering product-specific sessions provided almost all training on wound dressings. These sessions were useful for bite-sized educational refreshers and keeping up to date with new products.
‘So like someone comes in and does some education on a particular super-absorbent, it’s very specific to their product, it tells you like the pros and cons of that particular product, which is really useful, that does definitely inform my decision. But I think just generally we need more general training as well.’ District Nurse Sister, specific education group
The reduction in face-to-face teaching due to the Covid-19 pandemic had a negative impact on the consistent delivery of education.
‘’Before [the] COVID [-19 pandemic] we used to have reps come along quite frequently telling us about their products and what they have and it just gives you that refresher, because sometimes you can forget if you’re not told about it all the time.’ Community District Nurse, general and specific education group
Theme 2: project specific education
Dressing specific education
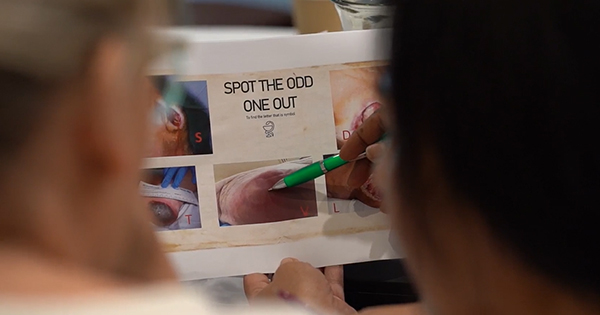
The dressing specific education was informative, providing a good understanding of the product, its scientific properties and usage. Being delivered over a lunch break fitted with staff schedules and a group session enabled them to discuss the dressing with colleagues, listen to others perspectives and ask questions. Understanding the ‘science’ and being able to handle the dressing was crucial to feel confident using the product in clinical practice.
‘She went through and obviously explained what it could be used for, would sort of then prevent us having to go and see these patients more often because I mean for us, anything that stops us being called out two, three times a week even…’ Community Staff Nurse, general and specific education group
‘Yeah I think when they passed it round as well and we could feel it, it felt quite high quality.’ Community District Nurse, specific education group
General education: the challenges in wound care course
The Challenges in Wound Care course provided new knowledge underpinning dressing choice and usage and promoted critical thinking. Some described how they (and their colleagues) often persist with the same dressing even when there is no obvious improvement to the patient’s wound, and the course made them ‘realise how many dressings are out there’.
‘Really good, really interesting and definitely made me sort of understand more, why I was making decisions I was and definitely made me more confident’ Community Staff Nurse, general and specific education group
The course was the first formal type of education some participants had received and they benefitted from the comprehensive structure of the modules. However, it was ‘too in-depth’ for some, who found it difficult to retain some of the detail and would have liked more time to complete the course.
‘I think some of it might have been a little bit too in-depth for my knowledge because obviously I’m not a Registered Nurse.’ Assistant Practitioner, general and specific education group
When asked if they felt the course was useful and helped their decision making, one participant described a common lack of general nursing knowledge around wound care and wound dressings:
‘When I was on the wards, no-one has a clue what they’re doing with wounds because especially on the ward I worked on, it was a really high turnover of patients, so everyone just guessed and made it up and we were probably putting some really inappropriate things on wounds.’ Community Staff Nurse, general and specific education group
The course, combined with the product-specific education supported clinical decision making more so than the product-specific education alone.
‘I think if you’ve got to have one or the other, it would be the Challenges in Wound Care short course.’ Community Staff Nurse, general and specific education group
Theme 3: impact of education on clinical practice
Some participants said they were experienced enough to trust their clinical judgement but that the dressing-specific education helped them trust the product through understanding how it was constructed.
‘It reiterated the indication of how much exudate a dressing can take before it would be changed and so that’s what I found helpful’ District Nurse Sister, specific education group
Others reported changes in clinical practice following education; one participant explained how clinical need was now prioritised over ritualistic practices.
‘I just thought if someone said oh this person’s dressing gets changed three times a week, I would just probably just have carried on and done it. But now, if I go and there’s like no strike through and it looks fine, I’m not going to change it for no reason.’ Community Staff Nurse, general and specific education group
Theme 4: usual wound care and wound dressing practice
Cultural and environmental factors determined why dressings were changed; some participants followed a specific treatment plan, whereas others optimised a dressing’s performance. Often, due to a lack of confidence, it was acknowledged that changing the culture of unnecessary dressing changes was needed.
‘I think a lot of, I think a lot of people in our team are a little bit cautious and change a dressing a little bit too frequently.’ District Nurse Sister, specific education group
Promoting change was challenging and several suggestions were made for how this might be supported. Pocket sized handouts or reference guides for staff to refer to during patient visits and an equivalent patient guide to help them understand the importance of avoiding unnecessary dressing changes were some of the ideas cited. Continued education was central to reinforcing this change.
‘I suppose sometimes it’s getting over that barrier of our traditional “we’ve got to go to this many times”, rather than actually looking at the dressing capacity and things. Because quite often we’ll get phone calls going “oh it’s leaking”, and when you get there you’re like no it’s not, that’s quite normal. So I think it’s probably changing our culture as such, that it’s quite okay to leave that dressing on because it’s not reached it’s capacity.’ District Nurse Team Lead, specific education group
Dressing changes and dressing choice
Reasons for dressing changes included clinical need (exudate/strikethrough), lack of confidence in the dressing/desire to see wound healing progression, patient schedule, lack of confidence/unwillingness to use own clinical judgement to change schedule and patient pressure to change dressing or the patient removed the dressing. Choice was often restricted through formulary but some staff still didn’t feel confident about choosing a wound dressing, or modifying a treatment regime set by another colleague. If a particular dressing was not promoting wound healing, it was common to rely on tissue viability nurses (TVNs) or senior nurses for advice.
‘I think it’s just a confidence thing and in a sense them not being confident to actually change a regime.’ District Nurse Team Lead, specific education group
Patient pressure and choice
The frequency of dressing changes was also influenced by patients; they ‘expected’ the nurses to visit on specific days for their dressing to be changed and often contacted the nursing team directly to report a dressing that had become displaced or a wound that was heavily exuding.
‘Patients will ring up and say like oh my dressing is leaking and it’s not, there’s just a little bit of…’ District Nurse Sister, specific education group
Education was key here, particularly product-specific education to enable participants to confidently explain to patients the dressing’s properties and the importance of leaving a dressing in place. This also suggests patient education (in the form of a leaflet or handout left with the patient during a visit) could further support this process.
‘I sort of explain it, they’re like driving a car, at the moment, your wound is healing up at seventy miles an hour, if I take that dressing off and it doesn’t need to, it’s like breaking your car and you have to build up speed again. So once I explain it like that, they understand and they’re happy with why I kept the dressing on.’ Community District Nurse, general and specific education group
Wound dressing expenses
Cost was important but clinical need and selecting a dressing that was ‘right’ for each patient was most influential in decision making.
‘I tend to always try to get what’s right for the patient. So maybe having a dressing is cheaper, but it’s not great for the skin integrity. So no I wouldn’t really think about cost…” Senior Community Nurse, general and specific education group
Discussion and conclusions
This study demonstrates the importance of continued education and learning opportunities for community nursing teams working within wound care, supporting the values of the RCN (2021) for continuing professional development in healthcare. A lack of previous wound care education was reflected in self-doubting behaviours where participants often sought reassurance from senior colleagues. This finding is consistent with previous research showing a lack of knowledge is related to feelings of incompetence (Moran and Byrne, 2018), whereas regular knowledge building reinforces confidence (McCluskey and McCarthy, 2012). Expense was not central in decision making for the participants in this study, who felt dressing selection should be based on clinical need. These findings are somewhat consistent with those of Gillespie et al (2014) who reported that acute care nurses in Australia relied on specialist nurses for support and guidance when caring for patients with wounds and they did not consider dressing cost a priority.
This study reinforces the importance of education to further knowledge, keep up to date with new products and developments and inform clinical practice. However, translating knowledge into action takes time and some participants in this study felt reluctant to change ingrained behaviours, demonstrating the need for regular education to reinforce good practice and avoid ritualistic practices (Welsh, 2018). General wound care, combined with product-specific education, was the most favoured approach for the participants; for many who lacked any previous form of structured education, general wound care education was essential to promote changes in clinical practice. Online learning provided an effective way of gaining new knowledge, and product-specific sessions formed an integral part of the nurse’s educational needs, facilitating a scientific understanding of how a dressing performed, which was essential for building trust in a dressing’s wound healing capabilities.
Indicative quantitative findings from this study suggest a possible benefit of the education package with dressing-related training. Reductions in overall wound dressing change frequency were observed in the group receiving the general and dressing-specific education package (mean dressing change frequency: 5.33 days) compared with the control group (mean dressing change frequency: 4.69 days), which corresponds to an increase of 13.6% in dressing change frequency. Similar improvements were also observed in mean wound dressing change frequency per patient between the two groups (6.00 days in the general and dressing-specific education group; 4.71 days in the standard care group), corresponding to an increase of 27.4% in dressing change frequency per patient. However, corresponding improvements were not observed in a comparison of standard care with the group receiving the product only training. This may have been a data artefact arising from the small numbers of patients and wounds featured in the study, which prevented definitive assessment of effectiveness.
Implications for practice
Wound care education, both product-specific and general education, is essential to ensure healthcare professionals feel confident in managing patients with hard-to-heal wounds, and regular training and education is key to encourage positive changes in practice. Product-specific education should demonstrate the scientific underpinning of the product and provide nurses with a solid understanding of how often a dressing should be changed and how to optimise wound healing to build trust in its usage. General wound care education that focuses on the core principles of wound management can help to build confidence and support positive changes in practice.
Directions for future research
This study has highlighted several important areas for future research to support healthcare professionals working in wound care. Future research should (I) explore the development of educational materials such as pocket sized booklets/reference guides for specific or general wound dressings for staff to consult during patient visits, (II) explore the development of patient-specific guides to support staff decision making and reinforce patient confidence and (III) explore the most appropriate forms of education to support nurse confidence in dressing selection and changes.