All patients are different and behind every wound is an individual (World Union of Wound Healing Societies, 2020a). Coloplast’s purpose is to make life easier for people living with wounds. They understand that wound healing can be complex; however, choosing the right solution doesn’t have to be. By combining effective products and services designed to release clinical capacity, reduce harm, and optimise services, Coloplast work with clinicians to reduce health inequalities and deliver optimal wound care for every patient.
In 2018, Coloplast highlighted the need to support Primary Care Networks to manage complex wounds. The Coloplast Wound Care Partnership Programme (WCPP) was created from this need. The WCPP aims to improve patient outcomes and increase cost-effective practices across primary care settings. This is achieved through the development and delivery of bespoke education, in addition to Tissue Viability Nurse Specialists (TVNSs) who help triage and ensure optimum patient management pathways.
‘Role modelling’ in wound care has a positive influence on systems and processes. There is a need for experienced staff to educate fellow clinicians. This in turn benefits practices and reduces the cost burden of wounds on NHS services (Wounds UK, 2018; Wounds International, 2020).
Coloplast Wound & Skin Care have invested in Tissue Viability Nursing services in the NHS over the past seven years to respond to the complexity and capacity challenges faced. Eight TVNSs were employed to support the implementation of Coloplast’s service programmes to deliver evidence-based education (Coloplast Professional), clinical support in practice and consultation in partnership with Integrated Care Board leaders, to respond to their local health challenges and ensure wound care services are tailored to their communities. Observations of the TVNSs in practice highlighted the need to understand the benefits of implementing The Coloplast 3 Step Approach framework to Assess, Prepare and Treat wounds. Anecdotal early findings, in clinical practice, demonstrated impressive results, therefore it was decided to formally evaluate and measure the impact of The Coloplast 3 Step Approach framework and products.
Two centres were involved in the first 60 patient evaluation. These were Hartlepool & Stockton Health in the Northeast of England and South Docs Services in Birmingham. All patients were seen by the Coloplast TVNSs within The Coloplast WCPP clinics. All data was collected in line with strict governance and data protection requirements, as documented in the service level agreement with the partnering organisations. Retrospective data were collected from electronic patient records and ongoing monitoring/reporting via Coloplast TVNSs, which was reported back to the partnering organisations.
The Complexity Spectrum
Many factors contribute to the complexity of a patient’s wound. Core contributing elements may vary in severity, but all have a role to play in the impact of a wound’s presentation and subsequent treatment. It is recognised that patient factors such as age, comorbidities, medications, concordance, economic status and gender play their part. Wound-related factors such as duration, size, wound bed condition and treatment response are also notable. The ability, attitudes and HCPs’ education will impact wound treatment and diagnosis, as well as the chosen treatment pathway. Lastly, if the resources available at the point of delivery, such as basic ankle brachial pressure index (ABPI) testing are not present and the HCPs ability to manage symptoms and associated problems is limited, then this will also have an impact on the complexity of the wound (Wounds UK, 2019). Being consistent with use of products and reducing the number of clinicians involved in dressing changes allows for greater progress and gives a better chance of effective monitoring of progress and evaluation of care in an objective manner (Guest et al, 2017).
What is The Coloplast 3 Step Approach?
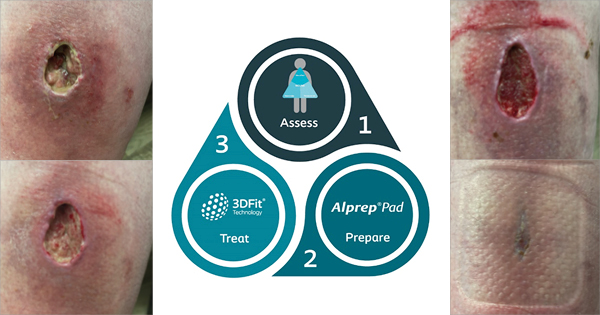
The Coloplast 3 Step Approach [Figure 1] is composed of three steps:
- Step 1: Assess — A holistic patient assessment including a full wound assessment is paramount in defining treatment objectives. Tools such as ‘The Triangle of Wound Assessment’ help identify issues in areas such as the wound bed, wound edge and periwound skin (Dowsett et al, 2015)
- Step 2: Prepare — Wound preparation is key to removing the barriers to healing, thus creating an optimum healing environment
- Step 3: Treat — The wound is treated according to the underlying aetiology and the specific treatment objectives identified at the assessment stage. A simplified portfolio of dressings is used to manage a wound of any depth and at any stage of healing.
Step 1: Assess
The Triangle of Wound Assessment
‘The Triangle of Wound Assessment’ is an evidence based holistic framework in which all areas of the wound (the wound bed, wound edge and the periwound skin) are assessed alongside the patient’s medical history, lifestyle, and social context. Each ‘zone’ of the wound, while interconnected, is treated as distinct and then assessed separately (Wounds International, 2016).
Wound bed
The wound bed is the most intensely monitored zone as it is often unpredictable. Signs of granulation tissue should be identified, while dead and devitalised tissue is removed. Exudate levels are managed and potential inflammation is reduced (Wounds International, 2016). Knowledge and understanding of AMS best practices should also be considered at this point (NICE, 2014; 2019; Wounds UK, 2020).
Wound edge
Barriers to healing at the wound edge should be lowered by debriding dried, thickened or keratotic edges, as well as macerated tissue. Exudate management should be improved to minimise risk of maceration (Wounds International, 2016).
Periwound skin
The skin within 4cm of the wound edge, as well as any skin under the dressing, is assessed for signs of maceration, excoriation, dryness, hyperkeratosis, callus and/or eczema, as well as skin stripping from adhesive products. The aim is to demarcate this area from the wound and reduce the risk of skin breakdown by protecting this area from exudate and/or moisture (Wounds International, 2016).
Step 2: Prepare
Alprep® Pad
Alprep® Pad (Coloplast Limited) is a two-in-one cleansing and debridement tool designed for improved exudate absorption and ease of use. The light grey or the dark grey side may be utilised first depending on the wound presentation.
- Two tools in one: The open structure of the dark grey foam is for loosening. The light grey softer foam is for absorbing and capturing debris, slough and exudate
- Designed for improved absorption: The unique slit design increases absorption and captures loosened slough, non-viable tissue and biofilms into the foam
- Ease of use: The ergonomic triangular shape makes for comfortable handling. The packaging can also be used to wet and hold the pad.
Alprep® Pad is suitable for a wide variety of wounds including non-infected wounds, infected wounds, or wounds with suspected biofilm. Alprep® Pad can be used by all clinicians treating wounds (Wounds UK, 2022).
Step 3: Treat
Appropriate dressings from the Coloplast portfolio, including Biatain® dressings with 3DFit Technology
Wound experts agree about the key factors for optimal exudate management. In Autumn 2019, wound care experts from around the globe gathered to discuss best practices in wound management. Ninety six percent of the group agreed that effective exudate management was one of the best ways to promote an optimal healing environment for both acute and chronic wounds. Managing the gap was agreed as important or very important for effective wound healing by 98%; 83% agreed that the best dressing choice for wounds up to 2cm deep is a dressing that conforms to the wound bed (Keast et al, 2020).
Biatain® dressings with 3DFit Technology conform to the wound bed to reduce exudate pooling and, thereby, reduce the risk of infection and maceration of the wound edge and periwound skin. These dressings:
- Absorb vertically to protect surrounding skin and wound edges from maceration
- Conform to the wound bed to minimise gap formation and reduce exudate pooling
- Retain exudate to reduce the risk of infection and damage to the periwound skin (Braunwarth and von Hallern, 2018).
Biatain® Silicone and Biatain® Silicone Ag with 3DFit Technology conform up to 2cm in depth*.
*in vitro, conformability may vary across product design
Methodology – One Simple Framework
In this study, 60 adult patients presenting with a variety of different wound aetiologies in a primary care setting were allocated to receive standardised care in the form of The Coloplast 3 Step Approach framework and the use of Alprep® Pad and Biatain® dressings as the solution for the ‘prepare’ and ‘treat’ stages. The patients were primarily reviewed by the Coloplast TVNSs with support from HCPs within the NHS practices. Following a comprehensive assessment, the preparation and treatment regimen was allocated, predominantly twice weekly. Patients continued to be reviewed until wound closure was achieved, or are ongoing in their evaluation through the partnering practices.
Due to the large number of patients with leg ulcers in the cohort (n=43), patients were stratified into 2 groups: simple and complex.
The literature [Box 1] demonstrated that there are multiple indeterminate definitions of what constitutes a complex leg ulcer. Therefore, for the purpose of this evaluation in the absence of a clear definition, a complex leg ulcer was defined by having one or more of the following:
- A wound surface area >100cm2 (10x10cm)
- Minimum duration of 6 months
- Not improved or reduced by 40% within 4 weeks despite following best practice
- Abnormal ABPI (outside 0.8–1.3 or unable to gain a reading)
- Current infection or history of infections
- History of non-concordance
- An active ulcer with one measurement between 2–6cm
- Comorbidities including peripheral arterial disease, diabetes, sickle cell, self-harm, intravenous drug use (IVDU), rheumatoid arthritis, immunocompromised and mobility restricted patients.
For the purposes of this evaluation, the core list of indicators above were used to further stratify complexity. Where a patient had 4 or more indicators present, patients were described as having increased complexity leg ulcers.
The Coloplast TVNSs were responsible for providing a holistic patient and wound assessment, wound preparation and treatment plan to the patients within the evaluation. The Coloplast TVNSs also provided mentorship and education to the practice nurses within the partnering areas, which allowed the upskilling of staff and support as needed for the evaluation. Healing progression was monitored using ‘The Triangle of Wound Assessment’ (Wounds International, 2016), which included wound tissue types and wound measurements. Pain was assessed using the numeric rating scale (NRS) both pre and post wound preparation. At the point of healing, patients were also asked to complete a patient satisfaction survey to capture impacts on their quality of life and experience. To further understand the patient’s experience, patients were also interviewed directly for their feedback.
Results
Faster Healing. Empowered Patients. Clinician Satisfaction
For all the wounds in the study (n=60), 85% healed; the remaining 15% were on a positive healing trajectory at publication. The average wound duration prior to implementation of The Coloplast 3 Step Approach was 55.2 weeks. The average healing time following implementation was 6.6 weeks.
Of these 60 patients, 17 presented with non-leg ulcer wounds of which 100% healed. The average wound duration prior to implementation of The Coloplast 3 Step Approach was 9.85 weeks; average healing time following implementation was 6.8 weeks.
There were 43 patients with leg ulcer wounds, simple venous leg ulcers (n=4) of which 100% healed; the average wound duration prior to implementation was 8.75 weeks; the average healing time following implementation was 3 weeks. Complex leg ulcers (n=32) of which 91% healed with an average healing time following implementation of 6.3 weeks, compared to 39.23 weeks wound duration prior to implementation of The Coloplast 3 Step Approach.
Patients who met more than 4 of the criteria for complex leg ulcers (patients with increased complexity leg ulcers; n=7) had wound reduction ranging between 13 and 85%. The average wound duration for this group of seven patients, with increased indicators of complexity, was 341.1 weeks prior to implementation of The Coloplast 3 Step Approach. One patient with more than 4 indicators of complexity healed in 26 weeks following implementation.
Seven patients (six from the increased complexity group and one patient with a complex leg ulcer who joined the evaluation after the initial cohort) are undergoing continued evaluation and are experiencing reductions in exudate, malodour, and pain. Reductions in slough and an increase in granulation and epithelial tissue has also been observed. Improvements have also been noted in patients with rolled edges and hypergranulation.
Of the cohort of the 60 patients, we have been able to simplify product choice for the treatment step of the framework utilising Biatain® dressings with 3DFit Technology (Biatain® Silicone, Biatain® Silicone Ag, Biatain® Non-Adhesive or Biatain® Ag Non-Adhesive) with 35 patients. Of the 35 patients, 88.5% healed within 6.2 weeks. As the evidence suggests, nearly 80% of wounds are less than 2cm in depth (Braunwarth and von Hallern, 2018), therefore, we anticipate that the numbers of patients eligible for a Biatain® dressing with 3DFit Technology could increase over the duration of the evaluation. In addition, no antibiotics were prescribed, demonstrating positive AMS.
Discussion
The results presented in this evaluation support the effectiveness of The Coloplast 3 Step Approach framework, and products, to provide an improved wound healing environment.
Across all patient groups, an improvement in average healing time was observed compared to wound duration prior to implementation of The Coloplast 3 Step Approach.
Parallels also need to be made to the National Wound Care Strategy programme (NWCSP) proposed healing expectancy of 75% of leg ulcers (uncomplicated with other conditions) healing within 24 weeks (NWCSP, 2023), and the Leg Club suggesting 67% of simple leg ulcers heal in 12 weeks (McIntyre et al, 2023). Promising results of 3 weeks to healing in the 4 patients with simple leg ulcers were achieved in this evaluation. By utilising a simplified framework, education and clinical specialist support, healing rates have demonstrated considerable reduction in the time to heal and positive patient outcomes.
As demonstrated following the preliminary literature review, it is acknowledged that further work is required to help clarify definitions for complex leg ulcers, due to the ambiguity and complexity of current working definitions. It was interesting to group data from the seven patients with four or more indicators for complexity and examine healing progress and expectation in this sub group. It is suggested this may be a more useful approach and may generate greater insight and understanding when evaluating wound care interventions in the future.
Good AMS practice is something all clinicians should be factoring into their chosen pathway of care. Treatments for wound infection that do not involve the use of antibiotics, antimicrobials or antiseptics are essential to promote AMS practices (WUWHS, 2020b).
Prior to the implementation of The Coloplast 3 Step Approach, 53.3% of the patients received antibiotics for their wound within a 6-month period prior to attending the WCPP clinic, with an average of 1.5 courses per patient. One patient had completed 48 courses of antibiotics as part of their previous wound management programme. No patients required antibiotics during The Coloplast 3 Step Approach evaluation.
Conclusion
Simplifying Wound Healing With The Coloplast 3 Step Approach
Whilst this evaluation demonstrated improved clinical outcomes, it is important to recognise that the intervention was comprised of 3 significant elements:
- All patients underwent a thorough and holistic wound assessment
- Care for all the patients was standardised and based on the use of The Coloplast 3 Step Approach and a simplified portfolio of Coloplast wound care products
- Overall full holistic patient and wound assessments were completed by the TVNSs; however, some care was provided by HCPs in the NHS practices, and patients were also involved in supported self-management.
Tools to encourage more patient involvement do not signal a reduction of care or a threat to the role of the clinician; instead, they focus on the importance of person-centred care which is supported by national and international guidance (e.g. World Health Organization, 2016).
This evaluation demonstrates that there are overall benefits for patients in terms of improved healing outcomes and quality of life by following a simplified framework and product choice – but also greater satisfaction for the clinician’s delivery of care. In addition, it has been demonstrated that The Coloplast 3 Step Approach ensures less antibiotic usage and promotes shorter healing times, as well as cost reductions to over burdened services.
Rising costs of healthcare, increasing numbers of people living with wounds and an understanding that patient wellbeing can be optimised are all drivers of greater patient engagement and involvement (Guest et al, 2017; Wounds International, 2016; WUWHS, 2020a). The Coloplast 3 Step Approach recognises that by ensuring appropriate preparation and treatment according to wound aetiology and condition that impediments to healing are reduced or removed. Best practice in holistic wound assessment has the potential to improve healing rates, reduce the physical, emotional and socioeconomic impact of wounds on patients. It also benefits practitioners and the NHS by reducing the overall burden of wounds, potentially decreasing workload and the costs associated with wound care. Furthermore, it raises practitioner and patient morale by improving patient outcomes (Wounds UK, 2018).