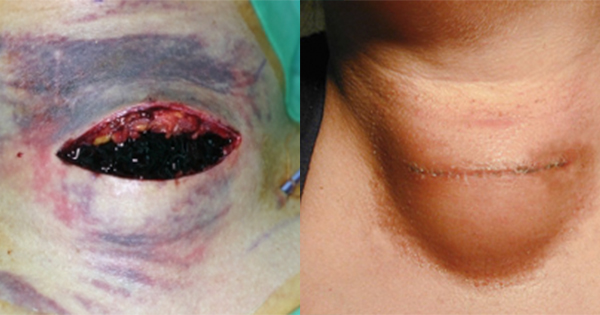
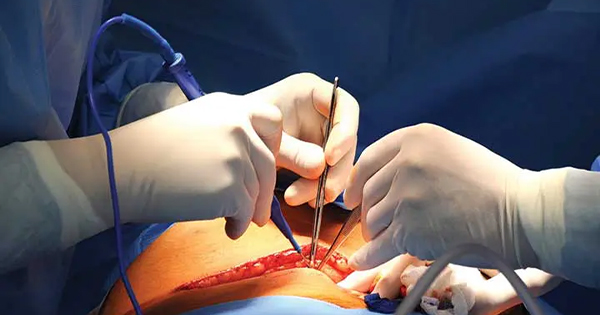
Surgical site infection (SSI) is a type of healthcare-associated infection, in which a surgical incision becomes infected within a 30-day period following surgery, or up to one year after surgery in patients receiving implants. SSI can be a devasting complication and cause significant morbidity and mortality if left untreated. Risk of SSI varies depending on the type of surgery, but have been shown to account for up to 16% of all healthcare-associated infections (NICE, 2013) and is the third most commonly reported healthcare-associated infection (Stryja et al, 2020). In 2017/2018, the NHS spent £8.3 billion on the management of an estimated 3.8 million patients with a wound across the UK, of which 14% (519,000) had a surgical wound; it was reported that only one-third of admissions attributable to surgical wounds and trauma appeared to be linked to a suspected infection (Guest et al, 2020). This article will explore the burden of SSI and its associated consequences, focusing on vascular patients, while highlighting the importance of preventative strategies and the value of using the new NICE pathway on preventing and treating SSI (NICE, 2021a). This includes new recommendations that Leukomed Sorbact (Essity) should be considered as an option for people with wounds that are expected to have low to moderate exudate after caesarean section and vascular surgery.