Regenerative medicine is the branch of medicine that focuses on the regeneration of damaged organs and tissues. It includes cell-based therapies, grafting or implantation of cells, gene therapy, and treatments based on growth factors and stem cells. Regenerative medicine is mainly applied to the following wounds:
- Wounds with loss of substance or risk of infection
- Suture or stoma dehiscence
- Abscesses and fistulas.
According to Pang et al (2017), wounds can be classified as acute or chronic. Acute wounds are those caused by surgery or trauma, typically healing within three weeks (Tottoli et al, 2020). The exudate from acute wounds is rich in leukocytes and nutrients. However, the acute healing process is susceptible to disruption or failure due to multiple factors that may affect all stages of healing (Bielefeld et al, 2013).
Surgical wounds are acute skin injuries resulting from surgical procedures conducted under sterile conditions, which are then left to heal by primary intention. They typically appear flat and are expected to heal without complications. Studies (Landén et al, 2016; Takagi et al, 2016) have indicated that while the inflammatory phase is crucial for controlling microbes, an imbalance in the cellular responses could lead to delayed wound healing. Primary intention healing may be delayed in the presence of infectious risk factors, such as when a drainage system is inserted.
Chronic or hard-to-heal wounds are characterised by a prolonged inflammatory response, persistent infection and lack of response to stimuli (Attinger et al, 2006); their exudate contains high levels of proteases and proinflammatory cytokines.
When the skin edges cannot be joined without excessive tension or there is tissue loss, a secondary intention healing process is preferred. The traditional management of such surgical wounds involves frequent dressing changes and packing of the wound cavity (Chetter et al, 2019).
Surgical wound dehiscence is attributed to various risk factors including age, sex, emergency procedures, type of surgery, postoperative cough and infection (Rucinski et al, 2001; Ceydeli et al, 2005; Van Ramshorst et al, 2010; Sandy-Hodgetts et al, 2013).
Traditional wound treatments aim to mitigate these risk factors and allow the normal healing process to progress towards scar formation (Pang et al, 2017), while regenerative strategies seek to achieve complete tissue regeneration and restore functionality (Schiavon et al, 2016). One such regenerative therapy involves the application of platelet-rich plasma (PRP), which accelerates the transition of the healing process from chronic to acute and promotes regeneration in traumatic and surgical injuries.
Platelet-rich plasma (PRP)
PRP is acquired through the centrifugation of whole blood, which separates other cells, resulting in a concentrated platelet solution in blood plasma. Platelet concentrates are categorised based on various parameters, including characteristics of the preparation kit, final volume, platelet concentration, preservation method, fibrin network architecture and preparation methods (Gibble et al, 1990; Harrison, 2018). PRP can further be classified as activated or non-activated, with activation achieved by adding substances such as calcium chloride, calcium gluconate or thrombin to produce a fibrin gel. Administration of PRP can be done through injection or topical application (Etulian, 2018).
Platelets have α-granules that contain primary growth factors necessary for tissue regeneration. These include transforming growth factor-beta (TGF-Β) 1, 2 and 3, vascular endothelial growth factor (VEGF), endothelial growth factors (EGF) and platelet-derived growth factor (PDGF).
Regulation of blood products
In Italy, the ‘Decree of the Blood,’ issued on November 2, 2015, and updated on August 1, 2019, establishes regulations to ensure the quality and safety parameters of blood and its components (Han et al, 2012). This decree governs the collection, storage, traceability and distribution of human blood and its derivatives, with regional authorities responsible for monitoring compliance. The law also stipulates specific requirements for platelet concentrate, including platelet and leukocyte concentrations of 1×106/µl ± 20% and <1×106/µl, respectively.
At our institution, we distribute various blood components for topical use, including autologous serum eyedrops, amniopatch for prelabour rupture of membrane cases with amniotic fluid leakage, and platelet gel (PRP and activator).
Aim
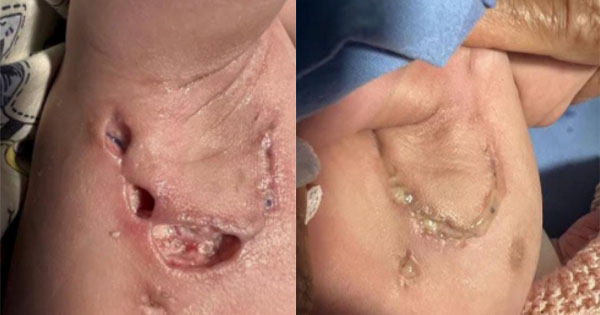
PRP, derived from human blood, can be used in the treatment of chronic or hard-to-heal wounds. In this case series, we describe the application of PRP in addressing challenging wounds in seven paediatric patients.
Case results
In the cases presented below, PRP was administered following wound bed preparation using advanced dressings or to aid in wound closure after negative pressure wound therapy. The application of PRP involved both injection and topical application around the periwound area, conducted in settings ranging from intensive care units to surgical wards and outpatient clinics. All of the local treatments described were supported by specific systemic antibiotic therapies.
The average duration between wound dehiscence and intervention was ten days (range: 6—60), with a median of nine days from dehiscence detection to the first PRP application (range: 0—21). The average interval between PRP applications was four days. Subsequently, all wounds achieved complete healing following at least two PRP applications, with an average treatment duration of 12 days (range: 8—18).
Ethics
Written informed consent was obtained from both parents and patients for the capture and use of photographs, taken before and after treatment, for all cases. Ethical approval was not required. Patient cases were reviewed in adherence to clinical protocols, and treatment was administered according to individual clinical needs.
Discussion
The use of PRP in wound healing was controversial in the past; however, emerging evidence supports PRP as a promising treatment modality for wound healing (Okudo et al, 2021). The positive outcomes associated with the use of PRP are due to the alteration of the pathological process, which is influenced by growth factors, leading to a visible change in wound appearance from chronic to acute.
Platelet gel effect consists of promoting appropriate granulation tissue for regeneration. Not only determines the recruitment of inflammatory cells which have a protective effect towards pathogens, but also determines the proliferation of soft tissue cells and this is proven particularly in traumatic wounds, both those caused by burns and those complicated due to local contamination (Menchisheva et al, 2019; dos Santos et al, 2021).
The clinical application of PRP was studied precisely for the good effects on tissue repair and regeneration. Evidence suggests PRP as a treatment strategy because the platelet-rich plasma has been shown to aid wound healing (dos Santos et al, 2021).PRP application is very widespread in the treatment of complex injuries of different aetiologies including diabetic foot ulcers, pressure ulcers, traumatic injuries, burns and infected wounds (Cetinkaya et al, 2018; Cieślik-Bielecka et al, 2018; Hirase T et al, 2018; Zhang et al, 2019; Okudo et al, 2021).
We could not find any evidence of the use of PRP in paediatric patients, however, our cases show that PRP is safe to use. The available studies on adult patients agreed that there are no treatment-related complications with PRP (Senet, 2003; Driver et al, 2009). There was one reported allergic reaction in a 14-year-old, which was a limited skin reaction to calcium citrate, used as an anticoagulant (Latalski et al, 2019).
As shown in our paediatric and neonatal cases, platelet gel use is effective in acute and chronic wound treatment or where healing could be prolonged.
Conclusion
While the concept of using PRP therapy has existed for many decades, its successful application, either alone or as part of adjunctive therapies, has only recently become evident. Currently, PRP remains unfamiliar to many healthcare professionals, potentially hindering patient access to this effective treatment for various conditions.
PRP has shown effectiveness in treating a range of complex lesions. In this series, we successfully treated seven cases of surgical wound dehiscence in a paediatric population.