Wound healing is usually referred to in four phases; haemostasis and inflammation, proliferation and remodelling (Almadaniet al, 2021). The main purpose of the inflammatory response is to prevent further blood loss by vasoconstriction, which results in a blood clot or scab (Ng, 2010). Fibroblasts play a key role in the proliferation phase leading to increased collagen production (Gibson et al, 2002). During proliferation new tissue is regenerated by fibroblasts, and during the final phase, remodelling, the newly healed wound forms a scar (Schultz et al, 2011; Sood et al, 2014).
Abnormal wound healing becomes evident when optimised local and systemic conditions are absent, leading to a ‘non ideal’ wound-healing environment (Cardinal et al, 2009). Hard-to-heal wounds, which can include pressure ulcers (PU), diabetic foot ulcers (DFU) and venous leg ulcers (VLU), are wounds where the skin and underlying tissues die due to ischaemia, infection, metabolic conditions, immunosuppression or radiation (Kuffler, 2021). Here we report a hard-to-heal scalp wound and the way in which it was managed and dressed.
Case presentation
A 53-year-old male patient who had a very painful ‘lump’ on his head for 6-week and was seen by the Oral and Maxillofacial team in A&E at the Royal Wolverhampton NHS Trust. The lesion started as a small ‘boil’, however by 6 weeks it had progressed to 7x7cm wound. He had three courses of antibiotics before presentation at our clinic, which were prescribed by A&E staff and his GP, these had not led to wound healing. The patient could not recall the names of the antibiotics.
On examination there was a 7x7cm crusted wound at the vertex (crown) of the scalp. The surrounding tissues were erythematous and tender. No pus was visible or obvious smell noted. No swabs were taken of the wound in A&E on the patients previous visit.
His medical history included; peripheral vascular disease, hypertension and diabetes. Due to Buerger’s disease he is a bilateral leg amputee. He smokes 12 cigarettes per day and has done for the past 40 years.
Investigations
The patient had incisional biopsies under local anesthetic two weeks after initial presentation to the Maxillofacial department. The histology report showed ulceration with underlying active chronic inflammation, with no evidence of malignancy. A CT scan was carried out that showed irregular scalp soft tissue thickening, no involvement of underlying bone and no other abnormalities.
Treatment
The patient was scheduled for debridement and further biopsies under general anaesthetic. The eschar was excised and sent for biopsies and pus was sent for microscopy, culture and sensitivity. The wound was debrided and irrigated with saline. Debridement of dead and inflamed tissue is key to prevent the formation of biofilms and infection in the wound. Debridement has long been recognised as a critical component for wound care and has been shown by several investigators to expedite healing (Steedt al, 1996; Cardinal et al, 2009). Flaminal Forte (Flen Pharma) was then applied, followed by Mepital (Molyncke) and Tegaderm (3M).
The histology from multiple biopsies came back as inflammation, with no evidence of malignancy. The pus culture grew Staphylococcus aureus sensitive to tetracycline and flucloxacillin.
The patient returned two days after the procedure complaining of pain from the anterior aspect of the wound and a foul smell. He was started on flucloxacillin 1g QDS and metronidazole 400mg TDS for 7 days. Microbiology was consulted who suggested Prontosan (B. Braun) soak to clean the wound, Flaminal forte, Atrauman (Hartmann) and a Softpore (Horsemen) dressing. We reviewed the patient 3 days after this and there were no complaints. The dressing was changed to Flaminal forte and Atrauman. The patient was then seen monthly for re-dressing, with no interim dressing changes.
Outcome and follow-up
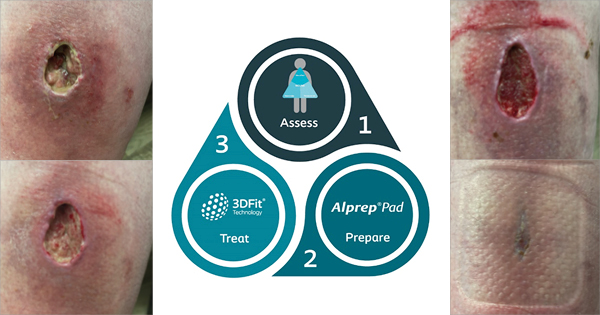
Following this the community district nurses have managed the patient with advice from tissue viability nurses. They advised Prontosan soak solution before dressing with Biatain Silicone Ag (Coloplast) border for continual antimicrobial and debridement of superficial slough and to change dressing as the exudate dictates. Figure 2–3 show the healing process.
Discussion
The annual prevalence of wounds increased by 71% between 2012/2013 and 2017/2018 (Guest et al, 2020). The number of acute and chronic wounds are increasing, highlighting the need for more discussion surrounding management and dressings.
These chronic hard-to-heal wounds usually arise as a result of poor blood circulation, diabetes or a weak immune system (InformedHealth.org, 2006). Smoking and diabetes strongly impair wound healing. Chronic wounds often occur in patients with diabetes mellitus (Spampinato et al, 2020). The patient was given smoking cessation advice but continued to smoke, although his diabetes was well controlled.
Following debridement, primary closure or local flap closure of the wound was not possible due to the size of the defect. Skin grafts are contraindicated in an infected wound bed (Elseth and Nunez Lopez, 2021). If the wound did not heal well by secondary intention, other options would have been considered.
This case was challenging to dress, as was a large area with exudate and infection. Initially after surgical debridement the wound was irrigated with saline and dressed with Flaminal forte followed by Mepital. Flaminal forte is hydrated alginate matrix embedded with a patented antimicrobial enzymatic complex. It is a good combination product that can be used in wounds when bioburden and exudate are clinical problems (White, 2014). Mepital is a dressing that does not adhere to a wound, promotes undisturbed healing and minimise pain at dressing changes (Barrett, 2012). However, it does not absorb exudate. Wound tissues should be physiologically moist, not dry but not wet. In any case where the wound is generating moderate-to-high levels of exudate, an absorbent dressing is needed (Ovington, 2007).
When the patient came in a few days later the wound was irrigated with Prontosan, a wound irrigation solution. The solution contains 2 active ingredients, an antimicrobial polyhexanide (polyhexamethylene biguanide [PHMB]), and a betaine surfactant (undecylenamidopropyl betaine; NICE, 2020). Studies show this has higher efficacy when compared with normal saline (Durant et al, 2014; Bellingeri et al, 2016). The wound was then dressed with Flaminal forte, Atrauman and Softpore. Atrauman is non-adherent and permeable to wound exudate (Stephen-Haynes, 2009).
The alteration of irrigation solution from saline to Prontosan and using Atrauman instead of Mepital, was effective in this case. Most cases reported in the literature like this one, are chronic wounds secondary to surgery or trauma, do not focus on the dressings used.
Conclusion
This case emphasised the importance of dressings and irrigation after surgical debridement. Although it took some time for the wound to heal, we achieved a good outcome and did not require any flaps for the wound closure. It healed by secondary intention and highlighted the importance of a multidisciplinary approach to care with valuable input from the tissue viability nurses, district nurses and microbiology team.