This article is based on a Made Easy workshop held at the Wounds UK Annual Conference in Harrogate, UK, on 6th November 2023. The workshop and this report were sponsored by HARTMANN. The focus of the workshop was on the Wound Balance concept, which aims to encourage a shift in clinicians’ focus from managing wounds to healing wounds whenever possible and as early as possible. Attendees of the session had backgrounds in a diverse range of settings, including community nursing, practice nursing, tissue viability, advanced practice and podiatry.
It was discussed how the Wound Balance concept can provide support with early intervention of immediate and necessary care, for venous leg ulcers (VLU) and lower limb wounds, and two case studies were presented. Towards the end of the workshop, the Wound-QoL tool (Blome et al, 2014) was introduced. This tool is an internationally validated questionnaire that aims to improve the patient journey by measuring quality of life (QoL) in patients with chronic wounds. A video was presented that delivered a first-hand account of a patient’s (Brian) experience of living with a leg ulcer, including how his family life and mental health have been affected. Attendees were provided with copies of the Wound-QoL questionnaire and were invited to consider Brian’s responses to determine how his wound has affected his QoL.
What is the ‘Wound Balance’ concept?
Wound Balance is a concept that aims to integrate various critical parameters which offer continuity, individualised care and support in clinical decision-making (Wounds International, 2023; Figure 1). By placing the patient at the centre of all care, the shift in focus moves from managing wounds to leveraging the clinical intention of healing wounds whenever possible and as early as possible. The Wound Balance approach aims to provide clinicians with the information to understand the science of wound healing, and how to balance the wound microenvironment to help patients get the best out of their treatments and, ultimately, improve clinical outcomes. During the session, it was stressed that identifying factors affecting wound healing is crucial to achieving Wound Balance, and that restoring the microclimate can help chronic wounds transition back into an acute-like state and towards a trajectory resembling wound healing [Figure 2]. These factors can be structured into three major areas:
- Wound Balance
- Patient Care Balance
- Clinical Practice Balance.
Why is there a need for ‘Wound Balance’?
Due to the growing number of individuals with chronic wounds, it is more important than ever that clinicians take the right approach to save time and utilise resources more effectively. In practice, there is often too much focus on managing wounds rather than healing them, and the Wound Balance concept can help give generalist nurses the confidence to deliver more effective care. Research has shown that there is unwarranted variation and inconsistencies in wound care delivery (Gray et al, 2019), and ritualistic practice is common with some clinicians being resistant to change. In some areas, services can be more clinician-led rather than patient-centred (Moore and Coggins, 2021), which may result in poor patient engagement and patients being wrongly labelled as non-compliant/concordant with treatment.
One way in which the Wound Balance concept can be implemented in practice is in conjunction with early intervention of VLU and lower limb wound care. Research has found that there is a lack of knowledge and practical skills among clinicians about VLU care and the application of compression therapy (Ylönen et al, 2014; Harding, 2016; Durán-Sáenz et al, 2022). It is estimated that over one million patients in the UK are affected by lower limb ulceration, which equates to 2% of the adult population (Guest et al, 2020). Moreover, the prevalence of VLUs in the UK has more than doubled from 2012/13 to 2017/18 (Guest et al, 2020). A further study by Guest and Fuller (2023) found that VLU healing rates in 2020 and 2021 decreased by 16% and 42%, respectively, compared with 2019 and time to heal increased by more than 85%. The direct costs associated with the care of individuals with VLUs by the National Health Service (NHS) in the UK have been estimated to be £7,706 per patient per year, which translates to an annual cost exceeding £2 billion when extrapolated to the UK population (Phillips et al, 2020).
Impact of venous leg ulcers (VLUs) on patients
Chronic wounds, such as VLUs, have a significant impact on patients’ QoL, including physical, mental and social aspects, leading to pain, anxiety, depression, poor self-esteem, disruption to social/work life and sleep disturbances (Kapp and Santamaria, 2017; Olsson and Friman, 2020; Folguera-Álvarez et al, 2022). It is widely acknowledged that QoL is often overlooked, and patients living with a chronic wound are not taken as seriously as those living with other chronic conditions (World Union of Wound Healing Societies [WUWHS], 2020; Wounds International, 2023). Although it can be challenging for clinicians to measure the psychosocial impact of VLUs on patients, it is important to note that reduced QoL can, in turn, negatively affect the wound healing process (Olsson and Friman, 2020).
Compression therapy for VLUs
Compression therapy is regarded as the mainstay, gold standard first-line treatment for patients with VLUs. However, compression therapy only treats the underlying symptoms of the disease by reducing venous hypertension and does not address the underlying aetiology, leading to cyclical manifestation. As a result, the National Institute for Health and Care Excellence (NICE) recommends that all patients with a VLU are referred to vascular services for assessment and consideration for endovenous ablation, in conjunction with compression therapy, to reduce the number of healing days (NICE, 2013; Gohel et al, 2018). However, research has found that 70% of patients with a newly diagnosed VLU are not referred to vascular services (Davies et al, 2019). In addition, research from Guest et al (2017) identified that 47% of UK practice is only achieving VLU healing rates at 12 months. These inconsistencies in VLU service delivery suggest that clinicians are just about able to manage wounds, let alone consider how they can heal them in the context of Wound Balance.
During the workshop, it was discussed how the concept of Wound Balance can be adopted in conjunction with the National Wound Care Strategy Programme (NWCSP) Leg Ulcer Recommendations (NWCSP, 2023). Recommendations from the NWCSP state that all patients presenting with a lower leg wound need to undergo a comprehensive assessment within 14 days. The NWCSP identifies the need for immediate and necessary care to be undertaken by any clinician attending to a patient presenting with a wound on the lower limb, whereby an initial assessment of any underlying red flags should be identified and escalated accordingly [Box 1]. The NWCSP recommends that clinicians clean the wound and its surrounding skin, apply emollient as required, apply simple, low-adherent dressings with sufficient absorbency and that they consider the following (NWCSP, 2023):
Patients without any formal assessment, palpation of pedal pulses or ankle brachial pressure index (ABPI), and at low risk of pressure damage of bony prominences, should be offered first-line mild graduated compression (20mmHg or less at the ankle)
Patients with red flag symptoms should not be offered compression as part of immediate and necessary care, and should be escalated for specialist advice accordingly. Following assessment and appropriate management by the relevant clinical specialist, compression therapy may be considered on a case-by-case basis.
A key take-away message from the session was that patients presenting without red flag symptoms need to go into graduated compression therapy of 20mmHg or less. When attendees were asked whether they were assessing red flags during the first assessment, it was found that the majority weren’t and that some clinicians are hesitant to put patients into compression therapy. It was stressed that omission of care is liable to no care and attendees were reminded that every chronic wound starts as a small wound. Therefore, the focus should be on wound healing rather than wound management by ‘nipping the wound in the bud’. The NWCSP provides clinicians with clear guidelines to instil confidence in them to deliver immediate and necessary care in the absence of red flags. Attendees were urged to seek support from companies or industry partners where appropriate – e.g. to help with running educational events. As long as both sides are open and transparent with each other, working with industry can be invaluable. A back-to-basics approach was also recommended alongside joined-up care delivery and interdisciplinary working, to ensure resources are used appropriately.
Early identification and intervention of patients with VLUs that require immediate and necessary care is key. As agreed by attendees, many complaints made by patients often boil down to a lack of communication between the patient and clinician. As a result, clinicians need to prioritise communication with patients to address their QoL needs. This can be improved through training and education to help improve clinicians’ skills. Opportunities for patients to self-care need to be considered and discussed with the patient to manage their expectations and address any concerns.
Superabsorbent polymer (SAP)-containing dressings and Wound Balance
Dressings are available to help achieve Wound Balance; for example, superabsorbent polymer (SAP)-containing dressings, which help address the wound healing environment and promote healing (Wounds International, 2023). SAP dressings, such as Zetuvit Plus Silicone Border (HARTMANN; Box 2) have been shown to effectively manage wounds with moderate to high volumes of exudate (Barrett et al, 2020), as they offer excellent absorption and retention of exudate, help to maintain optimal wound bed conditions, and sufficiently prevent leakage and other exudate-related complications (Hiskett, 2020). Moreover, there is evidence to show that treating hard-to-heal wounds with SAP-containing dressings results in a major shift in the pattern of biomarkers towards a trajectory resembling acute wound healing within 14 days, which persisted for 12 weeks (Mikosinski et al, 2022). Therefore, SAP-containing dressings have a key role to play in balancing biomarker patterns and improving patient QoL (Wounds International, 2023).
Case study 1
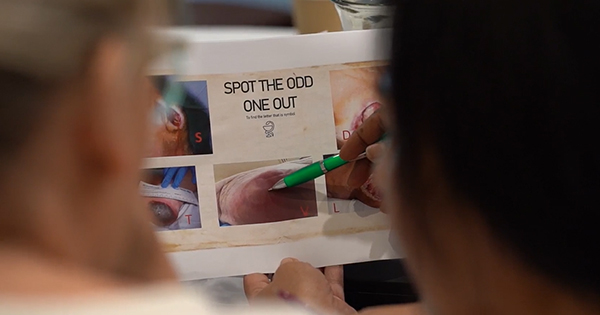
During the session, two case studies were presented where patients achieved improvements to their lower limb wounds following incorporation of early evidence-based intervention. The first patient was a 61-year-old female who presented to the urgent care centre after 3 months of self-caring for her wound. As the NWCSP (2023) recommends using a low-adherent dressing with sufficient absorbency, Zetuvit Plus Silicone Border was chosen in conjunction with first-line compression of 20mmHg. After a week of treatment, both exudate level and oedema to the surrounding limb had reduced. Following a full holistic assessment a week later, ABPI was deemed normal, and the patient was put into full compression therapy a week later. Three weeks later, the patient’s leg ulcer had completely healed [Figure 3]. A venous duplex scan was performed which showed significant reflux in the great saphenous vein and the patient was listed for endovenous ablation. In addition, consistent communication was maintained during their treatment to build up a good patient-clinician relationship and promote supported self-care to ensure the best outcome for the patient. The patient was also educated on signs that may indicate poor wound healing.
Case study 2
The second patient was an 81-year-old female who presented with a deteriorating wound caused by catching her leg on a car door. The patient also had reduced mobility and debilitating osteoarthritis of her knee, and had been on the waiting list for a knee replacement for 2 years. She was scheduled to have surgical intervention within 4 weeks; however, this had the potential for being delayed due to the patient’s open wound and the increased risk of surgical site infection. Therefore, the main goal of treatment was to focus on healing rather than managing the wound. After a week with Zetuvit Plus Silicone Border dressings and first-line compression hosiery, the wound had reduced in size by 50% [Figure 4]. The importance of taking a full holistic approach was emphasised; it is not in the patient’s best interests to keep them in the lowest compression class, and patients need to be reassessed within the 2-week timescale and their treatment plan adjusted according to their ABPI. Clinicians need to communicate with patients right at the start and make them aware that, where appropriate, the plan is to put them into full therapeutic compression therapy of at least 40mmHg to promote wound healing, and not to keep them in the lowest class. The patient’s wound healed within 4 weeks and her othopaedic surgery went ahead as planned. Early intervention had a significant impact on the patient’s QoL and helped ensure a positive treatment outcome.
The Wound-QoL tool
Living with a wound can have a severe impact on patient QoL and has a key role to play in all treatment (WUWHS, 2020). Although QoL is often difficult to quantify, there are specific wound-related QoL factors – that can have a substantial impact and cause anxiety or isolation (e.g. exudate/leakage and malodour) – that are not included in most patient QoL assessment tools.
The Wound-QoL questionnaire is a validated tool measuring QoL specific to wound care and the needs of the patient (Blome et al, 2014; Figure 5). It was developed based on three established disease-specific instruments: the Freiburg Life Quality Assessment for wounds, the Cardiff Wound Impact Schedule and the Würzburg Wound Score. The questionnaire includes 17 items that can be attributed to three subscales on everyday life, body and psyche, and the tool focuses on the patient’s experience within the past 7 days.
Listening to the patient and actively involving them in their own care and treatment can have a positive effect on wound healing, and tools such as the Wound-QoL questionnaire can help in practice. It is critical that treatment is needs-based and not just medically-based, so it is important to set realistic goals based on the patient’s needs and preferences. During the workshop, it was emphasised that clinicians need to take time to understand the patient and allow trust to be built, and that it can sometimes take multiple visits for patients to become fully invested in their care, instead of remaining passive recipients of care.
Patient quality of life
Only a handful of attendees shared that they currently undertake QoL assessments with patients. However, attendees agreed that tools, such as the Wound-QoL questionnaire, can give both the patient and clinician an opportunity to consider how living with a wound is impacting various aspects of the patient’s life. During the workshop, a video was shown titled ‘HARTMANN Story – Brian: Living with a leg ulcer’. Attendees were provided with copies of the Wound-QoL tool and were invited to tick boxes according to where Brian’s wound had affected his QoL.
Although Brian spoke about how he felt isolated and would avoid leaving the house for social activities, attendees noticed that Brian did not mention pain or how his sleep had been affected. It was widely agreed that pain is one of the most common complaints clinicians hear about from patients. Therefore, there was a consensus from attendees that the Wound-QoL tool is useful to help prompt clinicians to ask more specific questions and dig deeper.
After the video was shown, it was revealed that neither Brian nor his wife knew the impact that Brian’s wound was having on each other’s lives until they were asked the QoL questions – e.g. Brian’s wound had a knock-on effect on his wife, who would also avoid leaving the house and socialising. An important reflection from attendees was that clinicians tend to focus more on the patient rather than their family/carers, and that the Wound-QoL tool can help facilitate and improve conversations between everyone involved in the patient’s care.
It was concluded that if clinicians choose to utilise the tool in practice, they must take time to talk through the questionnaire with the patient. Clinicians need to avoid using the Wound-QoL tool as a tick-box exercise or filing it away in care plans. Assessments that consider QoL must be used actively to help clinicians determine how they can better support patients. Furthermore, patients need to be regularly reassessed to determine how their treatment is impacting their QoL and whether changes to their care plan are required.
Summary
During the workshop, it became apparent that some clinicians only classify wounds as chronic if they last longer than 2 weeks, with some clinicians sharing that they classify wounds much later. However, it was stressed that a shift in focus is needed – from managing wounds to leveraging the clinical intention of healing wounds – and clinicians need to conduct full holistic assessments and initiate interventions earlier. Early use of appropriate dressings, such as SAP-containing dressings, can help balance key biomarker patterns and achieve improvements in patient QoL. As reflected in the diverse clinical backgrounds of those in attendance at the workshop, the Wound Balance concept holds relevance for all healthcare professionals and has practical implications across a spectrum of healthcare practices and settings. The workshop concluded with a reminder to attendees that every chronic wound starts as a small wound, so it is critical that clinicians address issues in a timely manner and intervene at the earliest possible stage to prevent escalation of care. By actively involving patients in their care and asking them to express how they are feeling, clinicians can bring patients on board, and tools such as the Wound-QoL questionnaire can help improve patient engagement.