The authors conducted a retrospective caseload review to identify 30 patients treated with Flaminal® Hydro or Forte as the primary wound dressing. This review was carried out in one acute and one community healthcare setting in Ireland, with 15 patients selected from each setting, and the criteria for inclusion was any patient with a wound over the previous year that had been treated with Flaminal® Forte or Hydro as the primary wound dressing.
A variety of wound types were identified [Figure 1]. All patients in the acute setting (n=15) were treated with Flaminal® for non-healing postoperative wounds, with the primary aim of achieving complete wound closure. In the community setting (n=15), wound aetiology varied and included moisture damage, pressure ulcers and leg ulcers. There were three patients, each with one wound, where symptom management rather than complete wound closure was the primary objective.
Within each setting, the authors collected information on patient age and comorbidities, alongside specific wound aetiology, location and duration. The primary objectives of wound management were also recorded [Figure 2], along with documented pain scores and any verbally reported impacts on quality of life.
A standardised, internally designed data gathering tool was used in both the acute and community settings, using the patient’s case notes for completion. Wound outcomes were monitored and assessed over a 12-week period. The assessment included:
- Tissue type: This was routinely documented in each setting as part of ongoing wound assessments. Percentages of each tissue type, including necrosis, slough, granulation and epithelialisation, were assessed visually and noted. The authors used this data to track changes in tissue type throughout the 12-week period
- Moisture management: Levels of exudate, alongside frequency of dressing changes documented in the notes, were recorded. Any additional comments from clinicians regarding exudate levels were also noted
- Time to wound closure and percentage surface area reduction: Not all patients had accurately documented wound measurements; therefore, this parameter was subsequently removed. However, time to wound closure was noted
- Positive changes to quality of life: Pain severity using a visual analogue scale (VAS), where 0 indicates no pain and 10 represents the worst pain imaginable, as documented in patient files
- Other measurements included supported self-care and independence, as well as the documented impact on the patient. Additionally, any notable comments related to quality of life in the patient notes were recorded.
Results
Flaminal® in supporting primary objectives:
Pain
Pain was a challenge for all 30 patients, and reducing pain levels was documented as a primary objective in 53% (n=16). Six patient objectives focused on reducing general wound pain, while ten aimed to reduce pain during dressing changes. Analysis showed an average VAS score of 9.4/10 across the 30 patients prior to commencing Flaminal®. At the end of the 12-week period, this score had reduced to 0.6/10 [Figure 3]. Further analysis of patient-reported pain scores showed that after four weeks of treatment, VAS score had decreased by 6.9/10 to an average score of 2.3/10.
Debridement
Debridement was a primary objective for 63% of patients (n=19). Although this was not the primary objective for all patients, 90% of the healthcare professionals (HCPs) documented in patient notes that Flaminal® improved the removal of slough and necrosis [Figure 4].
This was further evidenced within the patient notes and recorded tissue types – a clear reduction in slough was noted, alongside an increase in granulation and/or epithelial tissues.
Managing bioburden
Managing bioburden was a primary objective for 27% (n=8) of patients. Signs of infection were documented in 40% (n=12) of patients, with descriptors including malodour, erythema, overgranulation and delayed wound healing. In two cases, the specific microbes were identified, including methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa. 7% of patients were on antibiotics (n=2). In all patients with reported infection, clinicians recorded a reduction in signs and symptoms of infection with Flaminal® use [Figure 5].
Exudate management
Exudate management was a primary objective in 50% of patients. The HCPs conducting this series reported that Flaminal® managed moisture well in all 30 cases, despite this not being a primary objective for every patient [Figure 6]. This is also evidenced by a review of dressing change frequency. Frequency varied depending on wound location and type, but for many, it was recorded as daily or on alternate days at the start of treatment, reducing to every 3–4 days. Of note, 17% (n=5) reduced dressing frequency after only two weeks of treatment, 15% (n=4) reduced dressing frequency after three weeks, and 10% (n=3) reduced dressing frequency after four weeks.
Enabling self-care
In this series, 70% of patients were able to either self-care with Flaminal® or share care with the HCP and family [Figure 7]. This led to reduced nursing time requirements and increased independence and wound management ownership for the patient.
Flaminal® in the acute setting (n=15):
The average wound duration prior to treatment was two weeks. The results of the treatment are as follows:
- 100% experienced improvements in slough/necrosis
- 100% found that Flaminal® managed moisture effectively
- 78% achieved full wound closure by week 12, while the remaining wounds were fully healed by week 18
- 100% experienced a reduction in pain, with all showing a marked improvement in VAS scores by weeks 2–3.
All patients included in the study had a positive experience. 85% of participants became independent in wound management throughout the treatment period, which led to written reports of increased independence and reduced anxiety.
Case studies in the acute setting
Consent was obtained from all patients in the following case studies to reproduce images and discuss their wound care.
Case 1
This case involves a 31-year-old male with recurrent pilonidal sinus disease. He presented with an acute wound post-second pilonidal sinus resection of the natal and intergluteal cleft [Figure 8a]. He had no significant comorbidities but had been previously non-concordant with treatment.
When asked to rate his pain using the VAS, he reported a score of 4/10. Although no clinical signs of infection were present, he was deemed high risk due to the wound’s anatomical location and moderate levels of exudate.
The objectives of the wound management strategy included promoting wound closure, managing potential bioburden reducing exudate.
Flaminal® Forte was applied daily and covered with a sterile gauze swab and foam dressing. After 10 days, the wound exhibited clear signs of improvement [Figure 8b]. By week 4 of treatment, wound dimensions had significantly reduced, and the VAS score decreased to 1/10; by week 6, it reached 0/10. Flaminal® successfully managed wound exudate and supported autolytic debridement. The wound remained infection-free throughout the treatment period and had fully healed by 7 weeks [Figure 8c].
Case 2
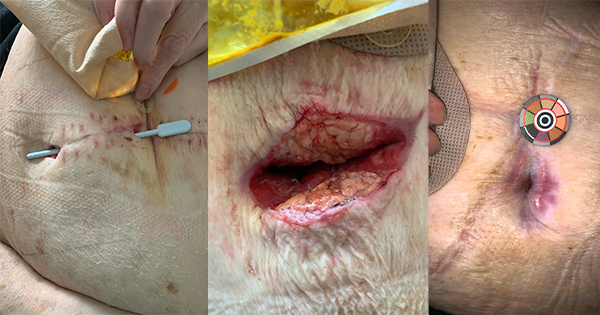
This case involves a 77-year-old male with surgical wound dehiscence of the perineum, post-laparoscopic abdominoperineal excision of the rectum [Figure 9a]. The patient has a medical history of ulcerative colitis, type 2 diabetes, hypertension and chronic renal impairment. The wound had been present for 15 days and was previously treated with a hydrofibre ribbon and topical negative pressure therapy with limited success. The wound was malodourous and deteriorating on presentation with moderate levels of exudate. Although no infection was suspected, the patient reported a pain score of 7/10 on the VAS scale.
The primary objectives of the wound management strategy included protecting the surrounding skin, debriding devitalised tissue, and reducing both odour and pain.
Flaminal® Hydro was applied, with secondary dressings of sterile gauze and silicone foam adhesive. Dressings were changed daily for the first two weeks and then every two days thereafter. After two weeks, the VAS score had reduced to 3/10. By week 7, the wound bed was clean with significant wound area reduction [Figure 9b], and VAS score continued to reduce. By week 6, the patient reported a pain score of 0/10 and remained pain-free. At week 11, only a small area of superficial granulation remained [Figure 9c].
Flaminal® Hydro had supported autolytic debridement, the malodour had reduced and the pain had reduced. Reducing pain was one of the patient’s primary objectives due to his inability to drive due to discomfort, leading to the need for friends or family to help with transport to hospital appointments. Two weeks after commencing Flaminal® Hydro, VAS score reduced to 3/10, and the patient was able to drive alone for appointments and play golf.
Flaminal® in the community setting (n=15):
The average wound duration prior to treatment was 4.5 weeks. The results of the treatment are as follows:
- 93% experienced improvements in slough/necrosis
- 100% found that Flaminal® managed moisture effectively
- 53% achieved full wound closure by week 12. Of those where wound healing was an objective, the remaining wounds had fully healed by week 24
- 100% experienced a reduction in pain, with the majority showing a marked improvement in VAS scores by weeks 2-3.
Pain was identified as having the greatest impact on individual patients’ quality of life. Consequently, reduced pain during dressing changes resulted in reported increases in independence, self-esteem, and mobility.
Case study in the community setting
Case 3
This case involves a 76-year-old female with a venous leg ulcer [Figure 10a]. The ulcer had been present for 8 weeks and was previously treated with silver. Initially, the patient reported a VAS score of 10, and standard care in the form of compression bandages was not tolerated. The wound was malodorous with evidence of Pseudomonas aeruginosa, but there were no signs of systemic infection. Exudate levels were high.
To reduce bacterial burden and cleanse the wound bed while managing high levels of exudate, Flaminal® Forte was applied as the primary dressing. This was covered with a superabsorbent secondary dressing and changed every two days. After three weeks, the VAS score had reduced to 7/10 and exudate levels had reduced [Figure 10b]. Compression bandaging was applied and dressing frequency was changed to every 3–4 days.
With the continued use of Flaminal® alongside compression therapy, the wound bed remained clean and granulating, demonstrating a 60% reduction in size by week 6 [Figure 10c]. The patient’s VAS score continued to improve, and by week 8, it was noted that having a dressing that does not cause stinging or pain, allowed this patient to tolerate compression bandaging, leading to full wound closure at 20 weeks.
Discussion
Wound progression and patient quality of life are closely interconnected. As wounds progress, whether towards healing or worsening, the effects on a patient’s quality of life can be profound. Slow or stalled wound healing is associated with increased pain, a higher risk of infection and reduced mobility. These factors directly influence a patient’s physical comfort and overall wellbeing. In contrast, when wounds progress toward healing, particularly when self-care is advocated, patients often experience improved physical function, less pain, and a general return to their normal routines, leading to a better quality of life.
A versatile wound dressing should effectively address various types of wounds and tissue types including acute, chronic, surgical and traumatic wounds. Addressing the specific needs of each wound and tissue type, including moisture, infection risk, and tissue integrity is vital to optimise patient outcomes in wound care. This case series demonstrates real world examples across an acute and community setting, of how Flaminal® Hydro and Flaminal® Forte can be integrated as simple wound treatment to address all these elements, achieving all primary objectives set by the specialist HCP.
This study demonstrates how Flaminal® not only aids in the physical healing of a variety of wounds, but also contributes to improved quality of life by addressing pain and discomfort. The impact of pain associated with wounds can be significant and multifaceted. Addressing pain is crucial for improving patient outcomes and enhancing overall management of wounds.
Conclusion
In conclusion, versatile wound dressings can assist patients to actively manage their healing whilst significantly reducing pain. These dressings not only promote optimal wound progression by maintaining a moist environment and protecting against infection but also provide enhanced comfort, minimizing discomfort and pain during the healing process.
As a versatile dressing, Flaminal® is a valuable option in wound care, helping to facilitate wound closure whilst addressing patient comfort. The need for a dressing that is simple to use but that can be used for a variety of wound types, tissue types and throughout different phases of healing can prevent the use of multiple combined dressings, thus having economic benefits for the health care system. For the patient and health care professional, a dressing that can be utilised to enable supported shared care and encourage faster outcomes of primary objectives can have a significant impact on patient quality of life.