Sharp debridement is the process of removing devitalised tissues from the surface of a wound typically using a scalpel or curette (Atkin, 2022). Sharp debridement is generally considered to be faster than autolytic approaches to debridement, for example, using honey, hydrogel or other moist dressings. This is due to the instantaneous nature of tissue removal during the procedure. Debridement of devitalised tissues is theorised to reduce the incidence of infection by removing dead tissues that might otherwise act as a medium for bacterial growth (Anghel et al 2016). The evidence of the benefits of debridement are not clear in terms of overall time-to-healing in wound types for which studies have been undertaken, such as leg ulcers (Gethin et al 2015). However, the potential reduction in the risks of infection and odour reduction resulting from the rapid removal of devitalised tissue makes timely removal of devitalised tissue a worthy element of wound management strategies.
The need for knowledge around the potential benefits and harms of sharp debridement is now included in the recently developed European Wound Management Associations (EWMA) level seven curriculum (Holloway et al, 2020) aimed at specialist health professionals in wound care. Organisations that provide training on wound care should therefore consider emphasising the importance of sharp debridement as an essential aspect of this area of practice. There is currently no regulation of wound care specialists in the UK so competencies relating to the clinical practice of sharp debridement is largely left to the judgement of individual practitioners as per the Nursing and Midwifery Councils Code of Conduct (2018) which states that “You work within the limits of your competence” (page 15). This ultimately leaves the judgement of what constitutes ‘competence’ at the discretion of practising nurses. Due to the lack of clear guidance around what constitutes competence in relation to the sharp debridement of wounds specifically, it is incumbent on the organisations responsible for delivering training on sharp debridement to provide a sufficient level of fidelity, with training processes to support such a judgement on the part of the learner. This should be accompanied, in addition, by appropriate supervision in a clinical context. It is also important to note that in some cases NHS trusts have developed in-house competency requirements to support health professionals to undertake sharp debridement. Without adequate support/training to perform sharp debridement, it is likely that nurses will avoid undertaking the procedure altogether. There are currently no data indicating the number of wound care specialists within the UK who perform sharp debridement on a regular basis or what their level of training was before starting to perform the procedure independently. If sharp debridement is not performed appropriately the risks include bleeding, destruction of important anatomical structures such as tendons and ligaments and pain (Anghel et al, 2016). These may be at the detriment to healing. It is therefore imperative that training on this procedure should re-create the conditions under which it is practiced as accurately as possible. For health professionals to develop a meaningful understanding of the challenges and risks of performing this procedure in practice. For example, when slough or necrosis is obscuring the presence of other structures or viable tissues within the wounded tissues.
Here we describe the development of a high-fidelity simulation aid to support training on sharp debridement within a higher education setting. The simulation aid was developed to support training provided on the tissue viability module run at the University of Salford.
Training aids currently used for sharp debridement
Currently approaches to providing training on sharp debridement outside of clinical settings have included the use of animal tissue (Bentley et al, 2005) and grapefruit-based models (Jackson and Rajbhandari, 2014). However, these approaches arguably lack functional fidelity (the dynamic interaction between the learner and the task), which is typically considered essential for learning psychomotor skills, such as sharp debridement (Carey and Rossler, 2021). In the case of contemporary simulation modalities for sharp debridement such as the use of grapefruit models or animal tissues, critical aspects of the functional experience cannot be simulated. These include:
- The placement of the wound to be debrided within a mannequin or wound model to simulate the functional challenges associated with debriding wounds in challenging anatomical locations
- Bleeding during debridement
- Changes in the mechanical characteristics of slough of necrosis within a wound
- The debridement of jellified haematoma tissue.
According to Carey and Rossler (2021) fidelity does not necessarily correlate directly with learning outcomes. They caution educators to consider the potential impacts of high-fidelity training aids, particularly for novice learners. This indicates that there are benefits to having a range of debridement models that provide training on this procedure. Low-fidelity models may be useful for developing basic practical skills with the use of scalpels and curettes. Whereas higher-fidelity models incorporating features that reflect the challenges of real-world debridement more closely may help develop confidence and competence further. The training aids described within this article can be used either as part of a desktop training exercise by placing the debridement model within a small wound model, or they could be built into a wearable silicone sheath model to allow learners to experience a higher-fidelity debridement experience where interaction with a human actor is a feature of the training.
The non-use of animal tissues, such as pork products, which may be unacceptable to some students due to religious beliefs is another benefit of this approach. It also does not require the generation of large amounts of organic waste or the need for refrigeration of training aids as is necessary for the use of animal tissue-based models.
Construction of the University of Salford training aids
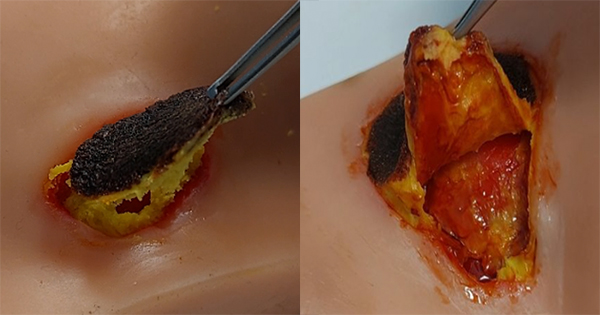
Necrotic pressure ulcer: (Figures 1–3)
This model takes around 10 minutes to produce.
Materials needed:
- Faux blood
- Vaseline (petroleum jelly)
- Talcum powder
- Yellow food colour
- Foam pad (black or soaked in brown food colouring)
- PVA glue (optional)
Construction:
- Construct the necrotic patch by cutting the foam pad into the shape and size of your model. You may need to trim the foam so that the scab is thinner (around 2mm thick).
- To create the slough mix 2/3 talc with 1/3 Petroleum Jelly (Add more talc for a thicker puss or more petroleum jelly for a slicker and softer puss) then add one to two drops of yellow food colour.
- Pack the puss mixture into wound cavity if you are using a pressure ulcer model as seen in the (Figure 4).
- Add faux blood over the top of the puss mixture
- Add puss mixture to the back of the scab foam and press firmly onto the slough mixture.
- Adding faux blood in very small amounts around the scab help to make the wound look inflamed and sore (Figure 5).
If you do not have a pressure ulcer model, modelling wax or silicone mixtures can be used to build up the skin and create a cavity for the wound to sit in. Then create the necrotic patch and slough filling as per the method above. Figures 1–3 illustrate this model.
Jellified haematoma wound
This model takes around 10 minutes to produce.
Materials needed:
- Faux Blood
- Vaseline (petroleum jelly)
- Talcum powder
- Yellow food colour
- Sterile film wound dressing
- Tea (from tea bag)
- PVA glue
Construction:
- Mix 2/3 talc with 1/3 Petroleum jelly (add more talc for thicker haematoma or more petroleum jelly for softer haematoma.
- Add 1–2 drops of brown food colour to a small amount of faux blood.
- Add tea and a small amount of PVA glue to blood mix to create a paste.
- Place paste mix onto the wound model and cover with a thin film wound dressing as in Figure 6
- Cover tissue paper with brown food colouring and faux blood, and place tissue paper over the wound film.
- The wound film will keep the haematoma mix and dry haematoma scab separate allowing the scab to dry fully.
Figure 7 illustrates the final wound model.
Conclusion
The clinicals skills training aids described in this article have the potential to improve simulation fidelity for students training to perform sharp wound debridement. The models described within this article are cheap and simple alternatives to traditional animal tissue or fruit-based training models for debridement. They offer an opportunity to not only improve the fidelity in relation to the mechanical properties of the wound tissues but can also be applied to a human actor using silicone sheaths to facilitate simulation of additional functional characteristics of the debridement process in real clinical contexts. The non-use of animal tissues, such as pork products, which may be unacceptable to some students due to religious beliefs is another benefit of this approach. It also does not require the generation of large amounts of organic waste or the need for refrigeration of training aids. It is hoped that a future evaluation of these training aids will indicate their relative value compared with previously described approaches to training on sharp debridement in relation to the confidence of practitioners to perform sharp debridement on patients who may benefit from the procedure. Future studies are needed to evaluate the pedagogical benefits of the different training modalities for this procedure and how this influences both clinicians’ competence and willingness to seek support to practice the procedure in clinical contexts