Infection as a barrier to healing
Wound infection is a major cause of delayed healing and may produce symptoms, such as malodour and pain, which distress patients and are a challenge for clinicians to manage (WUWHS, 2008). The cost of healing wounds that have become infected has been found to be up to several times higher than the cost of healing uninfected wounds (Driver and de Leon, 2008). In recent years, concerns about antibiotic resistance have stimulated widening usage of topical antimicrobial dressings, such as those containing silver or iodine, to manage wound infection. It is therefore essential that clinicians be able to identify wound infections correctly and, when appropriate, choose the right topical antimicrobial and/or systemic antibiotics for treatment, with the goals of preventing/eradicating infection to promote wound healing.
Identifying clinical signs and symptoms of wound infection
All wounds are contaminated with a variety of microorganisms (Stotts, 2004; WUWHS, 2008). In general, these microbes are harmless skin flora naturally found on the skin’s surface. Intact skin provides a physical barrier against these microbes. The creation of a wound, acute or chronic, damages this defence mechanism, letting microbes enter the body. Thus the presence of bacteria in a wound may result in increasing clinical problems along the continuum of infection, from contamination at the mild end, to systemic infection at the critical end (WUWHS, 2008).
Wounds generally require intervention when they reach the stage of localised infection, which is often characterised by pain, heat, swelling, redness and loss of function (WUWHS, 2008). To diagnose critical colonisation or local infection, clinicians must undertake and document a holistic assessment of the wound, including examination of the wound bed and periwound area, documenting any signs of redness, unexplained pain or malodour (Ousey and Cook, 2012). Other signs and symptoms of wound infection include purulent exudate, medium to high level of exudate and bleeding.
However, particularly in chronic wounds, a wound’s healing may be stalled despite the absence of obvious indicators (WUWHS, 2008). To ensure clinical diagnosis of infection, then, undertake thorough and regular holistic assessment and documentation of the wound so any deterioration is detected.
Need for early diagnosis and timely interventions
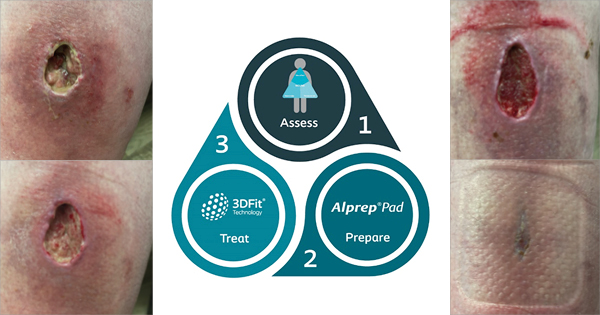
Prompt recognition and timely treatment of wound infection with a topical antimicrobial such as silver have the potential to reduce the economic, social and personal impact of delayed healing. However, effective management and treatment of wound infections is challenging, and wounds can improve or deteriorate over time, so timely recognition of any changes is essential (Wounds UK, 2013). Clinicians should therefore perform an initial wound and patient assessment, and regularly reassess to spot changes that might indicate wound infection or increased bacterial burden. The assessment should account for a number of factors, including those presented by the patient’s lifestyle (Box 1).
Further, wound assessment should account for considerations presented by the differences that manifest due to variations inherent in each wound aetiology. For example, in leg ulcers, it is particularly important to assess for and address underlying causes (eg superficial or deep vein incompetence), and refer patients to vascular services if the wound is not healed at two weeks (NICE, 2013). In addition, infection in the diabetic foot is often difficult to recognise, as up to 50% of infected DFUs will not present with the classical signs of redness, heat, swelling and pain due to neuropathy (Edmonds and Foster, 2006), poor blood supply or an immunocompromised patient. In the absence of pain or altered sensation, other, often more subtle, signs of infection might be visible and should not be ignored (Edmonds et al, 2004).
Once infection is recognised, the next challenge is to ensure that the wound and the infection are managed appropriately and effectively. In 2008, the World Union of Wound Healing Societies (WUWHS) published guidelines on the management of wound infection. These and more recently published guidelines include the appropriate use of topical antimicrobial dressings (WUWHS, 2008; Wounds UK, 2013). The guidelines recommend that, for wounds not showing improvement after 10–14 days of topical antimicrobial therapy, the patient and management approach should be re-evaluated.
The two–week challenge: silver’s role in managing wound infection
Despite the widespread use of silver as an antimicrobial agent, the exact mechanisms of action have not been fully determined (DTB, 2010). Silver ions are thought to affect multiple sites within a bacteria cell by binding to negatively charged cell components (eg the cell wall, DNA and RNA), disrupting the function of these cell elements and causing cell lysis and interference with electron transport, enzyme function and cell division (Lansdown, 2002). A recent consensus document on the use of silver dressings for treating wounds suggested an initial 14-day period could be seen as a two–week ‘challenge’ during which the efficacy of a silver dressing could be assessed (Wounds International, 2012) (Figure 1).
Evaluating the use of Silvercel® Non–Adherent
SILVERCEL Non–Adherent is an absorbent antimicrobial wound dressing for use in wounds that are moderately to heavily exuding, and infected or at an increased risk of infection. It is designed to absorb wound exudate and contains silver–coated fibres (X–STATIC®) that exhibit broad-spectrum antimicrobial activity (Lansdown, 2002). The dressing features an ethylene methyl acrylate outer film layer that uses EasyLIFT™ Precision Film technology. This outer porous layer is designed to keep the dressing from adhering to the wound or shedding fibres (Clark et al, 2009a), which can help reduce pain at dressing changes (Stephens et al, 2010) and associated patient discomfort and anxiety. The antimicrobial action of SILVERCEL Non–Adherent relies on the absorption of wound exudate into the dressing, ensuring the availability of positive silver ions. The dressing’s absorptive properties (Stephens et al, 2009; Clark et al, 2009b) help manage the increased exudate production often associated with infected wounds, while maintaining the moist wound environment that assists wound healing and protecting the surrounding skin from the potentially damaging effects of exudate (Fleur, 2009).
Laboratory tests show it is effective against many common wound pathogens, including meticillin–resistant Staphylococcus aureus, meticillin–resistant Staphylococcus epidermidis and vancomycin–resistant Enterococcus. It also prevents and disrupts biofilm (Clark et al, 2009c; McInroy et al, 2010).
In vitro assessment has shown the release of silver ions from SILVERCEL Non–Adherent is sustained for up to seven days, even when challenged with high levels of fluid (mimicking wound exudate) (Stephens et al, 2009). This is likely to be longer than the wear time of the dressing on an infected wound, but suggests the dressing could remain in situ for up to a week while maintaining antimicrobial efficacy.
A new, four–week, prospective, non–comparative evaluation has examined the effect of SILVERCEL Non–Adherent on signs and symptoms in infected wounds of a variety of aetiologies. The wounds involved were diverse and, often, complex infected wounds that had been referred for specialist wound care. Many of the patients had risk factors for delayed healing and infection. SILVERCEL Non–Adherent had a positive effect by the second assessment on all clinical criteria examined. Particularly notable were the overall reductions in the proportion of patients with malodour, purulent exudate or bleeding at dressing change, and in pain scores.
The positive effects on all criteria were apparent by the first assessment even though over 90% of wounds were considered still infected at that stage. This is not unexpected, because improvements in signs and symptoms are likely to precede reclassification of a wound as uninfected. In patients who continued the dressing beyond the second assessment, the positive changes continued for some clinical criteria (eg malodour and exudate descriptor) but generally were maintained at similar levels. This was despite continued reductions in the proportion of wounds that remained infected, perhaps suggesting that other wound–related factors were contributing to the signs and symptoms.
The six case studies presented on the following pages have been selected from the study evaluation. They describe the use of SILVERCEL Non–Adherent in a range of wound types, and demonstrate its positive effects with regard to wound infection and amelioration of signs and symptoms of wound infection over a two– to four–week period.