The use of an appropriate support surface is a key element of the prevention and management of pressure ulcers (NICE, 2005). However, the wide array of support surfaces available and the different technologies used can cause confusion. This how to guide aims to help clinicians choose the best support surface for a patients individual needs.
What is a support surface?
A support surface takes the weight of the patient when lying or sitting, and is intended to spread out (redistribute) the pressure exerted on the tissues in contact with that surface. The term support surface can apply to specialist beds, mattresses and mattress overlays, and also to chair and wheelchair cushions.
Why is pressure redistribution important?
Pressure is a major contributor to the development of pressure ulcers. If sufficiently high, pressure may reduce blood flow to the tissues, and cause direct damage to cells and tissues. Usually, the reduction in blood flow causes the patient to change position to relieve the pressure and allow blood to flow again. However, if the pressure is not relieved for some reason, eg the patient is unable to move, or has a loss of sensory function, the reduction in blood flow can damage skin and soft tissues. The damage may cause a pressure ulcer.
In addition to pressure, tissue damage may occur when sliding forces (shear) applied to the skin are increased. For example, shear may be increased when a patient slips down a bed or during repositioning. The friction between the patient and the support surface tends to hold the skin in place while deeper tissues are moved. This can reduce blood flow and damage tissues by crimping or closing blood vessels (International Review, 2010).
How does a support surface redistribute pressure?
The amount of pressure is related to the weight of the patient and the size of the contact area between the patient and the support surface. Support surfaces minimise pressure damage to tissues by redistributing the mechanical loads imposed on the skin and soft tissues due to patient immobility. Some support surfaces redistribute pressure by allowing the patient’s body to sink into them. As the patient sinks down, more of the patient’s body comes into contact with the support surface, so that the patient’s weight is spread over a larger area. This produces an overall reduction in the pressure placed on the tissues.
Other support surfaces intermittently remove pressure from some areas of the body, while maintaining pressure on others. The intermittent removal of pressure allows the tissues to recover before pressure is reapplied and another area is relieved.
Types of support surfaces
Support surfaces are available as integrated bed systems, mattresses that can be fitted onto standard bed frames, overlays that are placed over existing mattresses, and seat cushions. Support surfaces can be divided into two broad categories: reactive and active.
Reactive support surfaces
A reactive support surface changes load distribution only in response to a patient lying or sitting on it. It may be powered or unpowered. The patient is able to sink into the surface, thereby increasing the area of contact with the patient’s body and redistributing pressure. Examples include:
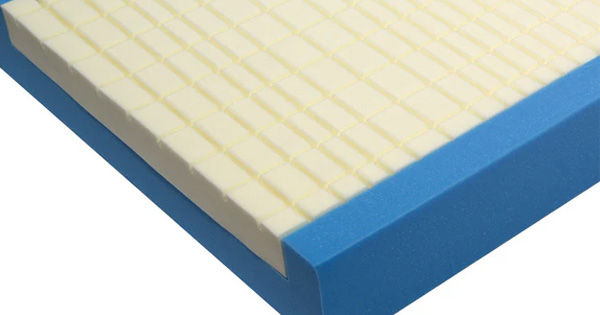
- Foam – mattresses composed of a block of foam or of layers of differing densities of foam. Foam degrades over time and may result in the patient sinking through it and onto the underlying support frame (known as ‘bottoming out’).
- Air- or gel-filled – surfaces comprise air or gel-filled compartments or columns.
- Low air loss support surfaces – some air-filled support surfaces allow air to escape through small holes. The air flows along the inside of a vapour permeable patient contact layer. This draws moisture and heat through the contact layer and away from the skin. This is known as ‘low air loss’ and may aid control of moisture on a patient’s skin (International Review, 2010).
- Air-fluidised support surfaces – contain sand-like particles, such as silica beads, through which air is forced. As the air is forced through the particles, they take on the properties of a liquid (ie become fluidised). The porous cover allows air to escape out of the mattress and body fluids to flow down into the support surface.
Active support surfaces
An active support surface can change its load distribution without a patient on it, and requires a power supply. Pressure is largely redistributed through the cyclical inflation and deflation of sections of the support surface so that pressure is removed from parts of the patient and then reapplied as other parts are relieved.
Alternating pressure surfaces are currently the only form of active support surface. Repositioning of patients is as important on active support surfaces as reactive surfaces (International Review, 2010).
When should a support surface be used?
Before deciding whether a patient needs a specialised support surface, clinical judgement should be used in conjunction with a comprehensive assessment that establishes:
- Risk of pressure ulcer development – as assessed by the score derived from a pressure ulcer risk assessment tool.
- Skin condition – including whether there is any existing pressure damage and whether the patient is continent.
- Level of mobility – level of assistance required to change position in bed and with transfers and walking, use of other equipment (eg a chair, recliners or wheelchair) that may require a specialist surface
- (eg mattress, seat pad, elbow elevation pads, suspension boots).
- Care setting and the patient’s and carers’ knowledge of using the support surface.
- Weight and nutritional status.
- Neurological status and co-morbidities.
The selection of a support surface should not be made on the basis of a score from a pressure ulcer risk assessment tool (NICE, 2005) or on the category of any pressure damage present (NPUAP/EPUAP, 2009) alone.
All patients vulnerable to pressure ulcers, should receive as a minimum, a high specification foam mattress. Active support surfaces are recommended for patients at greater risk of developing a pressure ulcer when manual repositioning is not possible (NPUAP/EPUAP, 2009).
Overlay or mattress?
Support surface overlays are positioned on top of the existing support surface to provide additional pressure redistribution. They have the advantages of being quick and easy to fit and not requiring the existing mattress to be removed and stored elsewhere. In a home-care setting, an overlay placed on one side of the bed may also allow partners to continue sharing the same bed. However, overlays may raise the total height of the bed making getting in and out of the bed more difficult, or cause safety issues if bed rails are in use. Also, Nixon et al (2006) identified that overlays could be more expensive than mattress replacements when overall costs were considered.
Choosing a support surface
Selection of an appropriate support surface should take into account risk factors for pressure ulceration as well as patient factors, ease of use and impact on nursing procedures. It is also important to take the views of patients and carers into account when selecting a support surface. However, decisions on which support surface to choose are often limited by availability and reimbursement issues. Continued research into the effectiveness of different support systems is required to assist with decisions
about reimbursement and funding (International Review, 2010).
Factors to CONSIDER when choosing a support surface
- Weight and size of the patient
- The weight limit of the support system should not be exceeded. Obese patients may need a bariatric support surface.
- Patients who are very light or small may not sink into a reactive surface sufficiently to produce adequate pressure redistribution.
- Some air-filled surfaces can be adjusted for patient weight.
Ease of use
- Is training required in the use of the surface?
- The length of time before the support surface is ready to use (ie is there an inflation time?).
- The support surface must fit the space for its intended use. Can it be transported to the space easily? Some integrated bed systems are unsuitable for home settings because of their bulk and weight and the need for a generator in case of loss of electrical power.
Maintenance
- How easy is the surface to clean and decontaminate?
- Does the support surface need specialist maintenance? Some support surfaces need to be taken off site for specialist cleaning between patients.
Impact on nursing procedures
- Some integrated bed systems include a ‘turn assist’ feature that helps with repositioning, examinations and linen changes.
- Overlays may raise a bed surface height to a level where bed rails no longer prevent falling, or cause difficulties for patients getting in/out of bed: if an overlay is required consider using a reduced-depth base mattress.
- If the support surface lacks a firm edge, a patient previously able to transfer/stand from the bed may no longer be able to.
- Some patients who are able to reposition themselves on a standard mattress might find that they are not able to do so on some support surfaces.
- A patient with a high level of skin moisture or who has a highly exuding wound may be best nursed on a low air loss or air-fluidised surface.
Microclimate
Support surfaces can influence the microclimate of a patient’s skin (eg foam mattresses tend to increase skin temperature and gel-filled products initially have a cooling effect but this wears off over time) so this must be taken into account when choosing a patient’s support surface.
Patient comfort and choice
- Some support surfaces make a noise during operation that may disrupt sleep.
- Some patients find the sensations produced by lying on some support surfaces disturbing or painful.
Once pressure redistribution strategies have been set in place, it is important to assess their effectiveness. Changes in the condition of the patient and their ongoing risk levels should be monitored as these may alter the prevention strategies required (International Review, 2010).
Role of a support surface in patient care
The use of a support surface is only one facet of the prevention and management of pressure ulcers. It is important that clinicians are fully trained in the use of any support surface and understand how its use fits into the wider care of a patient. Support surfaces should be used as part of a comprehensive care plan which incorporates ongoing reassessment and takes account of the patient’s needs and preferences (NICE, 2005).
Patients who are being cared for on support surfaces continue to need repositioning. The repositioning regimen (ie positions used and frequency of repositioning) should be documented and appropriate for the patient’s needs and ability to reposition themselves (NICE, 2005; International Review, 2010).
Quality drivers and pressure ulcers
Pressure ulcers are expensive to treat, with nursing time making up most of the cost. The other costs of treatment, eg dressings, antibiotics and pressure-relieving equipment, are relatively low (3.3% of the total cost) (Dealey et al, 2012).
As a result of the high costs of treatment, and because most pressure ulcers are avoidable, there is increasing emphasis by the UK government on prevention. One of the eight High Impact Actions for Nursing and Midwifery set out by the NHS Institute for Innovation and Improvement is ‘Your Skin Matters’. This initiative aims for there to be no avoidable pressure ulcers in NHS care (NHS Ins
titute for Innovation and Improvement, 2009). As a result, many NHS trusts in England are emphasising pressure ulcer prevention and have Commissioning for Quality and Innovation (CQUIN) targets for reducing the number of pressure ulcers (Morton, 2012). However, consistency and standardisation of pressure ulcer reporting are required nationally if meaningful comparisons are to be made between different geographical areas.
There is a continuing need for education in all aspects of prevention, categorisation and management of pressure ulcers across the health service, and with the current resources and capacity within the NHS this will be an ongoing challenge.
References
- Dealey C, Posnett J, Walker A (2012) The cost of pressure ulcers in the United Kingdom. J Wound Care 21(6): 261-266
- European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel (EPUAP/NPUAP) (2009) Prevention and treatment of pressure ulcers: quick reference guide. Washington DC: National Pressure Ulcer Advisory Panel; 2009. Available at: www.npuap.org/Final_Quick_Prevention_for_web_2010.pdf
- International Review (2010) Pressure ulcer prevention: pressure, shear, friction and microclimate in context. A consensus document. London: Wounds International. Available at: www.woundsinternational.com
- National Institute for Health and Clinical Excellence (2005). Pressure ulcers. The management of pressure ulcers in primary and secondary care. NCG 29. Manchester: NICE. Available at: www.nice.org.uk/cg29
- NHS Institute for Innovation and Improvement (2009) Your Skin Matters. Available at: www.institute.nhs.uk/building_capability/hia_supporting_info/your_skin_matters.html
- NHS Quality Improvement Scotland (2009) Best practice statement. Prevention and management of pressure ulcers. Edinburgh: NHS Quality Improvement Scotland, 2009. Available at: www.nhshealthquality.org
- Nixon J, Nelson EA, Cranny G, et al (2006) Pressure relieving support surfaces: a randomised evaluation. Health Technol Assess 10(22):iii-iv, ix-x, 1-163
- Morton N (2012) Preventing and managing heel pressure ulceration: an overview. Br J Community S18-22
Further reading
- Clark M (2009) Understanding support surfaces. Wounds International 2(3). Available at: http://www.woundsinternational.com/product-reviews/understanding-support-surfaces
- Fletcher F (2009) Pressure ulcer management – how to guide. Wounds UK 7(1). Available at: https://wounds-uk.com/pdf/content_10475.pdf
Contributors:
Liz Ovens, Clinical Service Lead Tissue Viability, Hillingdon Community Health and Central and North West London Foundation Trust