The prevalence of patients with chronic wounds continues to grow year-on-year and this places a substantial burden on health care resources. It is estimated that the NHS treats more than 2.2 million wounds annually, equating to 4.5% of the adult population, and the total cost of managing these wounds and associated co-morbidities is calculated to be £5.3 billon per year (Guest et al, 2015). However, it has been recognised that there are considerable unwarranted variations in wound care services across the UK and that standardising practices offers opportunities to improve healing rates, reduce patient suffering and provide cost efficiencies (NWCSP, 2020).
In 2019 the National Institute for Health and Care Excellence published medical technologies guidance in relation to the UrgoStart treatment range. The committee reviewed five empirical research papers, three of which were randomised controlled clinical trials. The committee critically appraised the publications and concluded that there was evidence to support the case for adopting the UrgoStart treatment range to treat patients with diabetic foot ulcers and venous leg ulcers in the NHS, as the use of the UrgoStart treatment range was found to be associated with increased rates of wound healing when compared with non-interactive dressings. Furthermore, they suggested that using the UrgoStart treatment range as part of the overall management of diabetic foot ulcers and venous leg ulcers could reduce costs for the NHS.
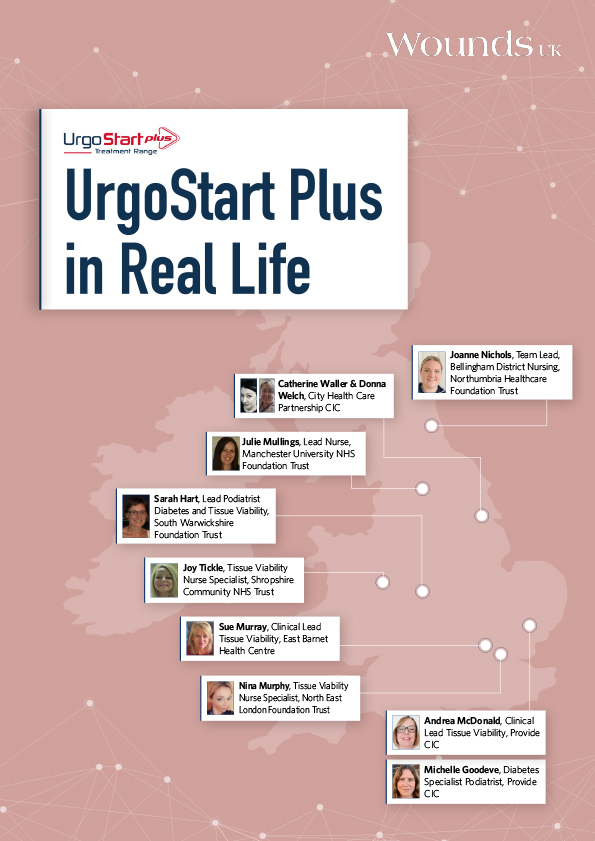
For many years, clinicians and academics have been calling for an increased focus on the need for high-quality evidence in relation to dressing therapy intervention, as we need to ensure treatments are worthwhile in terms of direct cost, clinical time and patient outcomes. High-quality empirical evidence and recommendations from NICE help standardise care, eliminating the unwarranted variations in practice. However, it is important to remember that the NHS measures quality in three key ways: patient safety, patient experience, and effectiveness of care. Research evidence provides the quality assurance in terms of patient safety and effectiveness of care, but what is equally important is the patient and clinician experience. This document showcases the real-world outcomes of the UrgoStart treatment range when implemented in practice, complementing its high level of evidence: demonstrating improvements in local healing rates, overall cost-saving, enhanced patient quality of life and enriched staff morale.
Clinicians and organisations need to ensure that all patients have equal access to appropriate therapeutic interventions, which are based on empirical evidence and should be used to inform local guidelines and pathways of care. Implementing evidence-based interventions optimises the patient’s potential to heal and ensures healthcare resources are used appropriately, therefore, increasing the likelihood of high-quality patient care and risk reduction.
Dr Leanne Atkin PhD MHSc RGN,
Vascular Nurse Consultant