Pressure ulcers (PUs) are a class of chronic wound and have been defined as “a localised area of skin and soft-tissue damage that usually occur over bony prominences, because of pressure or pressure in combination with shear” (European Pressure Ulcer Advisory Panel [EPUAP] et al, 2019). Although they can occur at any age, older patients are especially susceptible to experiencing a PU because of the physiological changes in the skin due to aging, as well as other factors that are more common with age, such as malnutrition, dehydration and reduced mobility (Ayello and Baranoski, 2004; Voegeli, 2007; Keevil and Kimpton, 2012). Certain risk factors also predispose individuals to developing a PU. For example, in a systematic review, Blackburn et al (2020) identified ischaemia, stress, recovery of blood flow, tissue hypoxia and the pathological impact of pressure and shear, as the main risk factors and underlying pathological mechanisms that interact in the development of PUs.
PUs are a costly problem for healthcare systems worldwide, with median prevalence rates in Europe being reported at 10.8% (Moore and Cowman, 2019). In the UK, PUs are estimated to cost the NHS £1.4 billion–£2.4 billion annually, due to a combination of the nursing time associated with their management, treatment costs and increased length of hospital stay (Wood et al, 2019). Data from NHS Digital (2022) on UK NHS Hospital Accident & Emergency Activity showed that over 1,300 new PUs were recorded each month between 2019-2020, affecting 200,000 people annually (Guest et al, 2017; NHS Digital, 2021).
In the US, it is estimated that 2.5 million cases of PUs are identified each year (National Pressure Injury Advisory Panel [NPIAP], 2019) with Padula and Delarmente (2019) finding that nursing costs associated with caring for these patients being around $50–100 per patient, per day. It is estimated that 2.5 million cases of PUs are identified each year in the US (National Pressure Injury Advisory Panel [NPIAP], 2019). High rates of PUs have also been identified in Australia, with evidence showing that PU are prevalent in up to 46% of care home residents, with incidence rates in up to 34% of residents (Hanhel et al, 2017).
PUs have significant negative impacts on patient quality of life (Moore and Cowman, 2009; Boyko et al, 2018) and are largely preventable. As such, strategies to reduce their development including the use of a risk assessment tool, visual and physical inspections of the skin and tissue by a healthcare professional, and regular repositioning (EPUAP et al, 2019) are some of the most commonly used methods of prevention. These subjective measures of risk are often used in combination with objective approaches to treatment and prevention including laser and electromagnetic therapy, which uses an electrical field to stimulate healing (Machado et al, 2017), and support surfaces (EPUAP et al, 2019).
Support surfaces for pressure ulcer prevention
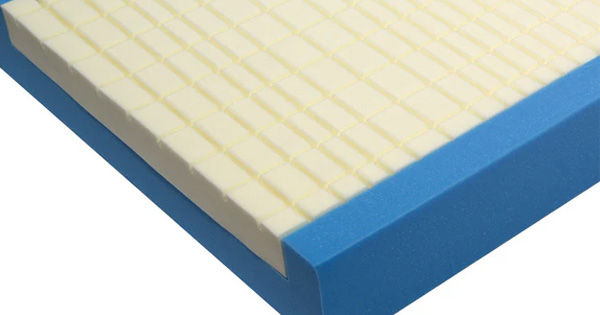
International guidelines for the prevention and management recommend PUs should be managed using a risk assessment tool, regular repositioning, skin and nutritional care, and the use of support surfaces. Such support surfaces should be selected based on the patient’s level of mobility, shear reduction, location of PU and risk of developing a new PU (NPIAP, 2019). Support surfaces, such as integrated bed systems and mattresses are designed to redistribute pressure on the body to increase blood flow (Wounds International, 2010) and can be powered or non-powered; the latter using reactive pressure redistribution to relieve pressure and can include alternating pressure (active) air surfaces, reactive air surfaces, foam surfaces and alternative reactive support surfaces that are made neither of foam materials nor air cells (NPIAP, 2019).
Although the NPIAP (2019) guidelines suggest using “a high specification reactive single layer foam mattress or overlay in preference to a foam mattress without high specification qualities for individuals at risk of developing pressure injuries,” there is a lack of evidence if such support surfaces are clinically and cost effective (Bhattacharya and Mishra, 2015), with decisions about their use usually based on a multitude of variables (Beeckman et al, 2013).
In a Cochrane review that included 32 studies and 9,058 participants, exploring the effects of alternating pressure (active) air beds, overlays or mattresses compared with any support surface in PU prevention, there was little difference between an alternating pressure air surfaces or foam surfaces in reducing PUs (Engkasan, 2023). Similarly, Shi et al (2021a) assessed the effects of alternating pressure (active) air surfaces compared with support surfaces on PU incidence and found that from 32 randomised controlled trials (RCTs) that were included in the review, it could not be concluded that alternating pressure mattresses reduced PUs compared to foam surfaces.
It was also unclear if there was a difference in the number of people developing new PUs when being treated on an alternating pressure air surface, and reactive water-filled, fibre, air, gel or standard hospital surfaces.
In another review by Shi et al (2021b) assessing the effects of beds, overlays and mattresses on PU healing in people with PUs of any stage, in any setting, from 13 studies which included 12 two-armed RCTs using a parallel group design, and one trial-based economic evaluation, and 972 participants from acute, community and long-term care settings, the authors concluded that there was uncertainty of the impact of pressure-relieving mattresses in a variety of comparisons, including alternating pressure (active) air surfaces versus foam surfaces; reactive air surfaces versus foam surfaces; reactive water surfaces versus foam surfaces, and a comparison between two types of alternating pressure (active) air surfaces. However, the authors stated that patients who were nursed on reactive air surfaces were more likely to have their PUs completely healed over a 37.5-day follow-up than those nursed on foam mattresses.
In a systematic review to assess the effects of foam beds, mattresses or overlays compared with any support surface on the incidence of PUs, Shi et al (2021c) found that from a total of 29 studies (9,566 participants), there was little difference in PU incidence in people treated on foam mattresses compared to other types of support surfaces including reactive fibre surfaces, reactive gel and foam surfaces and other types of foam surfaces. In a further review to summarise the evidence from six Cochrane reviews, Shi et al (2021e) concluded that the evidence suggests compared with foam surfaces, reactive air surfaces, alternating pressure air surfaces and reactive gel surfaces may reduce PU risk and increase wound healing, with reactive gel surfaces possibly being more effective in operating rooms and long-term care facilities.
However, the authors did report that some studies included in the review had methodological limitations (such as small sample sizes and inaccurate or incomplete descriptions of their methodologies) which could have had an impact on their overall findings.
Despite a large amount of research exploring of the impact of pressure-relieving mattresses on PU prevention, it remains unclear if pressure-relieving mattresses have a positive impact on PU prevention. This review aimed to explore the effectiveness of pressure-relieving mattresses in PU prevention.
Methods
Embase and MEDLINE were searched for relevant published literature between 2018 and 2023. Search terms focused on the effectiveness and cost effectiveness of pressure redistribution mattresses on PUs. Table 1 shows the search strategy.
Inclusion and exclusion criteria were used for assessing the relevance and inclusion of the studies in the review [Table 2].
Results
The search identified a total of 11 records. Nine studies were excluded for not meeting the inclusion criteria. The two remaining studies were included in the review (Beeckman et al, 2019; Nixon et al, 2019). Both studies used an RCT study design.
Main themes
Two main themes were identified from the results. These included PU prevention and management and cost-effectiveness.
Pressure ulcer prevention and management
PU prevention and management was the focus of both studies included in this review, with the studies comparing the effects of different types of mattresses in PU prevention with a standard care control group.
The study by Nixon et al (2019) explored the time to developing a new category 2 PU in a sample of 2,029 patients who were randomised to be nursed on either an alternating pressure mattress (intervention; n=1,016) or a high-specification foam mattress (control; (n=1,013). The participants were recruited from 42 secondary and community inpatient facilities in the UK and were considered to be at high risk of developing a PU. Participants were involved in the treatment phase of the study for a maximum of 60 days, with follow-up taking place in the final 30 days. Results showed there was insufficient evidence that one mattress was significantly better than the other in preventing PUs with no group differences observed. The median time to develop a PU was 18 days in the intervention group compared to 12 days in the control group, with 160 and 124 new PUs of category >2 being observed in the different groups, respectively.
The study by Beeckman et al (2019) compared the effectiveness of static air support surfaces and alternating air pressure support surfaces in a Belgian nursing home population consisting of 26 nursing homes (96 wards) and 208 participants who were recruited through convenience sampling. Participants were randomised to either the intervention group, where they were nursed on static air support surfaces or support surfaces that were not standardised in current clinical practice (control group). In this study, the static air mattress was found to be significantly more effective than an alternating air pressure mattress in preventing PUs with a lower incidence of category II–IV PUs in the intervention group than in the control group. The time to develop a PU was also significantly longer in the intervention group, with the median time being 10.5 days compared to 5.4 days in the control group.
Cost-effectiveness
Beeckman et al (2019) concluded that static air mattresses were more cost-effective than alternating air pressure mattresses, mainly due to their longevity. This study found that mean healthcare costs from using an alternating pressure mattress were lower than when using a high specification foam mattress with the authors suggesting that alternating pressure mattress had a 99% probability of being cost-effective. However, the cost analysis in this study was performed using information from the purchase costs and longevity of the mattresses rather than a full cost-effectiveness analysis.
Nixon et al (2019) found a small, but insignificant, cost-saving benefit in favour of alternating pressure mattresses.
Discussion
This review explored the effectiveness of pressure-relieving mattresses in PU prevention. Two studies meeting the inclusion criteria were included in the review. The main themes of PU prevention and management and cost effectiveness were investigated with mixed findings. While Nixon et al (2019) reported insufficient evidence that alternating pressure mattress were better than high specification foam mattresses in preventing PUs in a high-risk group of patients, Beeckman et al (2019), when comparing the effectiveness of static air support surfaces and alternating air pressure support surfaces in a nursing home population, reported that static air mattress were significantly more effective than an alternating air pressure mattress for prevention.
The conflicting findings in these studies could be attributable to different patient populations (nursing home patients compared to high-risk patients in secondary and community inpatient facilities), as well as the different follow-up periods – 14 days in Beeckman et al (2019) compared to a maximum of 60 days (with follow-up in the final 30 days) in Nixon et al (2019). Indeed, Beeckman et al (2019) suggested that future studies should incorporate longer follow-up in light of evidence that demonstrated time to develop a PU was 16 days (Serraes and Beeckman, 2016).
Both studies also compared different types of pressure-relieving equipment. Alternating pressure mattresses were used in the Nixon et al (2019) study and compared with high specification foam. Both static air support surfaces and alternating air pressure support surfaces were used in the intervention group by Beeckman et al (2019). The alternating support surfaces used by patients in the control group in this study were not standardised, meaning there could have been a difference in the incidence of PU in the control group using different types of support surfaces, although the authors did not analyse these differences. These methodological differences mean it is difficult to accurately conclude the effectiveness of pressure-relieving mattresses on PU prevention, which has also been highlighted in the literature. For example, Jiang et al (2014) and Malbrain et al (2010) suggested that there is no difference in PU healing rates between patients nursed on alternating pressure mattresses or static air mattresses.
Sauvage et al (2017) reported that alternating pressure mattresses were better than Visco foam mattresses, but the study suffered from high dropout rates and methodological limitations. Jiang et al, (2020) reported a higher incidence of PUs in patients using alternating pressure mattresses compared to Visco foam, but the repositioning schedule of patients varied, meaning it is difficult to draw accurate conclusions from the data. Furthermore, In a quality improvement study using Visco foam and 12 self-adjusting air bladders for patients at risk of developing a PU in a 275-bed hospital, there was a 66% reduction in stage III and IV hospital-acquired PUs, suggesting that such devices offer a benefit over standard care (Elsabrout et al, 2018).
Both studies included in this review reported on the cost effectiveness of pressure-relieving mattresses compared to usual care; however, these results were also mixed. Although Beeckman et al (2019) concluded that static air mattresses were more cost-effective than alternating air pressure mattresses, Nixon et al (2019) reported that alternating pressure mattresses were more cost effective, although this finding was not significant. However, in the Beeckman et al (2019) study, cost analysis was performed using information from the purchase costs and longevity of the mattresses rather than a full cost-effectiveness analysis, which could account for the conflicting results.
These findings reflect the current literature, which is also inconclusive. For example, the systematic review by Shi et al (2021a) reported that alternating pressure air surfaces are more cost-effective than foam surfaces for preventing PUs. In another review, Shi et al (2021b) suggested that reactive air surfaces possibly cost more than foam surfaces per day for patients who do not have a PU. In a further review, Shi et al (2021c) reported that alternating pressure mattress are probably more cost effective than foam surfaces.
In the quality improvement study by Elsabrout et al (2018), cost savings of $714,724 were reported when using Visco foam and 12 self-adjusting air bladders for patients most at risk of developing a PU. Engkasan (2023) reported a small cost-saving benefit to using alternating pressure (active) air beds, overlays or mattresses compared with foam mattresses. Serraes and Beeckman (2018) reported no significant difference in purchase costs of standard hospital mattresses compared to a foam or viscoelastic foam mattress. It is interesting to note that much of the evidence surrounding cost effectiveness is obtained from the acute hospital perspective and with an aging and frail population, it is essential that the overall cost to the healthcare system, including the cost of such mattresses being used in a domestic setting, is also explored.
One important factor not explored in both studies included in this review is patient comfort and quality of life. While Beeckman et al (2019) did not explore this caveat, Nixon et al (2019) did report a small benefit in patient comfort in favour of alternating pressure mattresses, although the researchers highlighted the need for patient preference to be accounted for when decisions about mattress choice are made. Other evidence suggests it is unclear if there are any differences in patients’ comfort, adverse events or quality of life between different types of support surfaces for PU prevention, largely due to a lack of reported patient outcomes (Shi et al. 2021a, 2021c). Engkasan (2023) also concluded that there was limited evidence to suggest a difference the comfort of different types of mattresses, quality of life or the occurrence of adverse events. However, Elsabrout et al (2018) reported a 50% reduction in patient complaints about mattress comfort in their quality improvement project, when using Visco foam and 12 self-adjusting air bladders for patients most at risk of developing a PU, suggesting the latter offered a comfort benefit over other types of mattresses.
Conclusion
Despite recommendations to use pressure-relieving mattresses to support PU prevention, the evidence to date is inconclusive about the most effective type of support surface and the benefits of using such devices for PU prevention and management, and patient comfort. Uncertainty about the cost-effectiveness of such devices also remains an important area of exploration.
Future research should focus on a standardised approach to measuring patient outcomes to further understanding of how pressure-relieving devices can help PU treatment and management. With an aging population and a transition to more care being delivered in the community setting, understanding the cost implications of using pressure-relieving mattresses in PU prevention is also an important area for future research.