Patients often report that relentless wound pain is one of the most challenging aspects of living with a hard-to-heal wound. Severe or moderate wound pain can significantly impact wellbeing, disrupt sleep patterns, make movement difficult and contribute to anxiety and depression (Hellström et al, 2016).
Pain is frequently cited as one of the main reasons why patients refuse or fail to engage with a range of gold standard treatments, including debridement and compression therapy. Although pain medications are widely prescribed, they are often ineffective and can lead to side effects such as drowsiness and an increased risk of falls. To reduce the burden of hard-to-heal wounds, non-pharmacological treatments are needed that can both relieve wound pain and promote healing.
This article is based on a symposium held at the European Wound Management Association conference in May 2024. The symposium focused on the use of microcurrent electrical stimulation therapy (EST) as a non-pharmacological approach to accelerate healing and reduce pain in hard-to-heal wounds, particularly lower limb wounds.
Three key speakers—Dr Amelia Swift, Reader in Healthcare Professional Education at the University of Birmingham; Spencer James, an expert in wound care; and Maria Moon, Senior Research Nurse at Home Wound Care International—discussed how using microcurrent EST, specifically the Accel-Heal Solo electrical stimulation device, can support patients with venous leg ulcers (VLUs) and lower limb wounds.
Progression of chronic pain
Amelia Swift gave an overview of the progression of chronic wound pain. It begins with nociceptive pain, which is caused by tissue damage, inflammation and heightened sensitivity during the healing process. If this pain persists and becomes severe, it can evolve into neuropathic pain, resulting from nerve damage. This type of pain affects up to 58% of people with leg ulcers (Eusen et al, 2016). The combination of both nociceptive and neuropathic pain ultimately contributes to the development of chronic pain.
Impact of pain
Amelia then outlined the impact of pain in three key areas: physical, psychological and social, all of which affect a patient’s quality of life.
Physical impacts to be considered include wound odour, which can cause embarrassment and discomfort for the patient, functional restrictions as a direct consequence of the wound and disrupted sleep from either pain or pain-relief medications. Additionally, falls may occur as a result of restricted mobility or due to the unsteadiness and fatigue caused by some analgesics, particularly opiate-based ones.
The psychological impact of pain leads to feelings of powerlessness, hopelessness and emotional stress. As a consequence of chronic pain and the physical impacts of unhealed wounds, disruptions to daily living occur. For example, patients may be unable to fulfil caregiving roles for their partner or grandchildren. They may avoid socialising due to concerns about wound odour, fatigue from lack of sleep or side effects of pharmacological analgesics. As a result, patients often focus on coping with their wound pain rather than living as they would in a pain-free scenario.
From a social perspective, chronic wound pain can lead to loss of work, social isolation and feelings of loneliness, which may develop into anxiety, depression and low self-esteem.
Challenges of chronic wound care
Amelia identified three key areas that represent the biggest challenges in the successful treatment of hard-to-heal wounds and pain management.
1. Budgetary challenges
Wound care costs the NHS £8.3 billion a year (Guest et al, 2020), of which £5 billion is needed to manage hard-to-heal wounds. To put this into perspective, obesity costs the NHS £6.1 billion and diabetes £10 billion per year (Department of Health and Social Care, 2017; NHS, 2022). Wound care products account for only 6% of total wound care expenditure, while appointments make up 53% of the annual costs (Guest et al, 2020).
2. Compliance challenges
There are several issues that practitioners and patients must address when treating chronic wounds. Up to 80% of people with a VLU experience background wound pain (Leren et al, 2020). Pain is a significant symptom for 50% of individuals with multiple leg ulcers, including those resulting from trauma (Sabah et al, 2024). This persistent pain can reduce patient engagement due to a perceived lack of progress. Furthermore, 44% of patients are unable to tolerate full compression dressings as a result of wound pain (Briggs, 2006). This, in turn, leads to nurses avoiding compression due to the associated discomfort (Atkin and Martin, 2020), leaving the wound unhealed.
3. Social and clinical challenges
Effective pain management and wound healing are closely connected; when pain is not well controlled, it can hinder the healing process (Milne et al, 2021). Chronic pain reduces patients’ quality of life and their engagement with treatment, increasing the risk of infection, amputation and higher care costs. Traditionally, the focus has been on managing wounds rather than healing them. With more individuals affected by chronic wounds, it is important for clinicians to use resources more effectively and consider approaches like EST to improve outcomes.
Electrical stimulation therapy (EST)
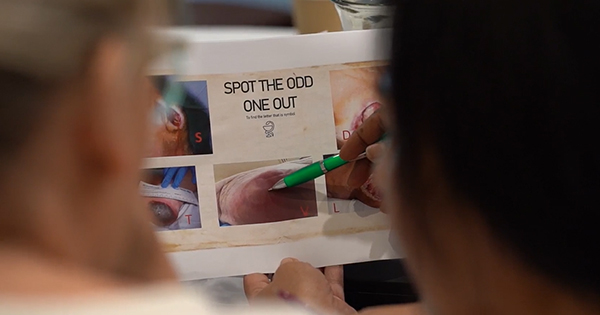
Electrical stimulation can be considered a ‘catch-all’ phrase for many different functional therapies and stimuli. It works by restoring the electrical current across the wound, encouraging the cells involved in healing to resume their normal functions [Figure 1]. It harnesses bioelectrical signalling, creating a positive feedback loop that alters cell behaviour at the wound site. EST promotes wound healing by stimulating various processes such as fibroblast proliferation and migration, re-epithelialisation, granulation tissue formation, collagen synthesis and growth factor production (Khouri et al, 2017). A forest plot analysing 15 studies demonstrates the differences in healing outcomes between wounds treated with standard wound care alone and those treated with standard care plus EST (Koel and Houghton, 2014; Figure 2).
In addition to promoting healing, EST reduces wound pain, providing a positive alternative to traditional pain management with pharmacological analgesics such as paracetamol, ibuprofen, opioids and gabapentin. Clinical trials [Figure 3] have demonstrated significant reductions in both pain and wound size with EST use, which helps increase patient engagement and supports recovery.
However, some EST devices, like transcutaneous electrical nerve stimulation (TENS), can cause pain and discomfort during the stimulation process because their stimulation is strong enough to activate sensory nerves, leading to muscle twitches or uncomfortable sensations similar to pins and needles (Draper et al, 2012). These devices with higher stimulation levels are also often not well-tolerated and are not recommended for use on open wounds (Atkin et al, 2019).
Dr Swift highlighted the importance of choosing the right electrical stimulation parameters, noting that painful stimulation from stronger devices can decrease patient engagement with the therapy and hinder wound healing. This underscores the need for portable and easy-to-use microcurrent devices (with stimulation levels 1000-fold less than TENS), such as Accel-Heal, which enable clinicians and nurses to deliver more effective care with confidence.
Accel-Heal Solo Therapy
Accel-Heal Solo [Figure 4] is a one-off, 12-day therapy that delivers a precise, targeted level of electrical energy to the wound. It can be easily incorporated into clinical practice and has two main benefits: promoting healing and improving pain management, particularly for patients with chronic pain where analgesics are ineffective.
The therapy is sub-sensory, meaning it uses a level of stimulation that the patient cannot feel, so it doesn’t cause any painful or tingling sensations.
Accel-Heal Solo delivers automatic, pulsed electrical stimulation via electrode pads that are placed away from the wound while still providing a positive impact on healing and pain reduction. These pads can be left on for up to 12 days, eliminating the need for frequent dressing changes and reducing discomfort and inconvenience. Additionally, the wound will continue to heal at an accelerated pace even after the treatment period ends.
Accel-Heal Solo: First-hand experience
During the symposium, Spencer James shared his personal experience with a hard-to-heal wound that began in his teenage years after being bitten by an insect on his leg, which developed into a leg ulcer. Despite six years of various treatments—including skin grafts, four-layer bandaging, and compression stockings—nothing had worked. Spencer was struggling with his quality of life due to the wound and the ongoing pain. Eventually, the wound healed, but keeping it healed became an issue.
Spencer decided to try Accel-Heal Solo after discovering videos about it online. He obtained a device, and the results were immediate. The pain relief was instant, and he noted that the integrity of the healing was better than anything he’d previously experienced. Spencer also stated, “I’ve now tried the product four times, on four separate wounds, and each time it’s led to incredibly rapid healing… as a patient, it’s changed my life.” In a video shown during the symposium, he further explained, “The thing about this product is that you don’t even know it’s on. It’s completely pain-free… the device is really easy to use, and it’s extremely wearable… there is no discomfort.”
Real-world studies
Maria Moon presented findings from a trial using Accel-Heal Solo. As a nurse specialising in wound care, Maria recognised the severe impact that unresolved pain has on patients’ lives and sought to assess the device’s effectiveness, particularly in terms of pain relief.
Microcurrent EST is a non-pharmaceutical option that has been shown to help relieve pain in hard-to-heal wounds as well as initiate healing (Arora et al, 2020; Chen et al, 2020; Avendaño-Coy et al, 2022). Maria wanted to determine if Accel-Heal Solo could deliver these benefits to her patients.
A service evaluation was designed to test the device’s efficacy and to see if it could positively impact patients’ pain. The study evaluated the use of Accel-Heal Solo to reduce pain associated with hard-to-heal wounds and its impact on the reliance on analgesics.
Methodology
Twenty patients were recruited for the study, all of whom had chronic venous or arterial leg ulcers and were experiencing moderate to severe pain that remained unresolved despite using various analgesics. The median duration of their wound was twelve months. The cohort was 75% female, with an average age of 74 years. Common comorbidities among the group included anxiety/depression, hypertension, high cholesterol, and arthritis.
The nurses applied Accel-Heal Solo which delivered a pre-set programme of sub-sensory microcurrents over a 12-day treatment period, during which patients were asked to record their pain scores and analgesic consumption. To establish a robust baseline, patients also completed a pain and analgesic diary daily for the seven days preceding the treatment. Following the treatment period, patients returned to regular NHS services but continued to provide pain scores to the evaluation team for an additional six months to assess any longer-term healing and pain-related outcomes. However, analgesic consumption was not formally monitored after the treatment phase.
Results
Reduction in wound pain
The study found that the mean wound pain score decreased from 5.8 out of a maximum of 10 (range 4.0–7.3) at baseline to 3.6 (range 0–6.0) after treatment. Key findings included:
- 50% of patients reported a shift to a lower pain category during the treatment period
- All three patients with severe pain at baseline moved to a lower pain category by the end of the treatment period
- The median reduction in pain, as measured on the numeric rating scale (0–10), was two points
- The median time to achieve a 50% reduction in baseline wound pain was 5 weeks (range 2–16) after starting treatment
- The median time to reach mild wound pain was also five weeks (range 1–10).
2. Reduction in analgesic intake
The study showed that the median daily dose was reduced for some analgesics:
- Paracetamol (n=14); 4000mg to 1500mg
- Ibuprofen (n=4); 600mg to 0mg
- Gabapentin (n=4); 750mg to 350mg
- Morphine; no changes were recorded for the two patients taking this analgesic.
The results indicated a clear reduction in pain for all participants, which was associated with a decrease in the use of pharmacological analgesics. In the opinion of the attending healthcare professionals, this reduction in analgesic consumption led to improved patient engagement, quality of life and sleep quality. These improvements, in turn, supported the overall wound healing process.
3. Improvement in wound healing
The study showed that Accel-Heal Solo resulted in an average reduction of 41% in the baseline wound area during the 12-day treatment period. Additionally, the mean weekly reduction in wound area from baseline to week four was 10.2% (range 0–24.6%; SD 6.2). Fifty percent of patients achieved healing within six months of starting EST, with the median time to healing being 18 weeks [Figure 5]. Among those who achieved healing, most reached full wound closure between weeks 8 and 14 following the start of Accel-Heal Solo treatment.
Case studies
Maria went on to present two case studies from the evaluation study that highlighted patients who had achieved both healing and pain reduction for their VLUs following the use of Accel-Heal Solo. She described how the device had positively impacted their quality of life and discussed the economic considerations of conventional treatment pathways compared to the use of Accel-Heal Solo.
Case study 1. Pain-free and fully healed within six weeks
A 67-year-old female patient presented with a VLU that had persisted for ten months [Figure 6a]. Her pain was severe, with a score of 9 out of 10. She was receiving daily gabapentin at a dose of 600mg, along with intermittent tramadol.
The patient began using Accel-Heal Solo and responded exceptionally well to the device. Her pain score decreased significantly from the first day of treatment, and her intake of analgesics was reduced accordingly.
By two weeks, the wound had reduced in size [Figure 6b], and by the end of four weeks [Figure 6c], she had ceased all analgesic use.
Although this aspect was not part of the formal study, Maria highlighted the health economics associated with the patient’s experience. Prior to using Accel-Heal Solo, the patient had endured ten months of regular dressing changes, multiple courses of antibiotics, a referral to a specialist department, ongoing analgesic consumption and complications due to sensitivity to morphine. This included two ambulance call-outs following adverse reactions to medication prescribed by her GP. These issues, common among patients with hard-to-heal wounds, have significant cost implications for the NHS.
The use of Accel-Heal Solo resulted in the patient being pain-free within 5 weeks and fully healed within six weeks.
Case study 2. Requested amputation to pain-free in three months
A 68-year-old female patient presented with a VLU that had persisted for 6 years [Figure 7a]. Her pain was severe, with a score of 8 out of 10. She was receiving daily paracetamol at a dose of 3000–4000mg, along with 1200–1600mg of ibuprofen.
The patient was an active grandmother and took her grandchildren to school every day. Due to the severe impact of the pain on her quality of life, she had even discussed the possibility of leg amputation. She could not tolerate thorough wound cleansing, debridement, Doppler assessments, or compression therapy. Additionally, managing her VLU had involved six years of frequent wound dressings (up to three times a week), multiple courses of antibiotics, and continuous analgesic use. Additionally, she had tried a single-use negative pressure wound therapy dressing, which was ineffective.
Within two weeks of using Accel-Heal Solo, her pain score decreased from 8 to 4, allowing her to tolerate Doppler assessments and compression bandages. By weeks three and four, the wound had improved in size and appearance [Figures 7b and c]. By three months, the wound was fully healed, and she was pain-free.
Conclusion
Unhealed wounds are a huge burden to the NHS costing over £5 billion per year (Guest et al, 2020). Time and money are spent on unproductive wound dressings, clinician time as well as regular antibiotic and analgesic consumption. Patients are suffering and painful non-healing wounds affect their quality of life, mobility and ability to engage with treatment.
Microcurrent EST offers an effective solution to poor healing outcomes and debilitating wound pain. It is supported by a high-quality evidence base and is rooted in fundamental biological processes.
Accel-Heal Solo delivers microcurrent EST in a convenient, easy-to-use format that provides great patient outcomes. Accel-Heal Solo makes it possible to adopt microcurrent EST across different types of care settings for the treatment of chronic wounds. It is easy to use, can be used alongside current topical treatments, is available ‘off the shelf’ and cost-effective, requiring no additional training.
As a result of using Accel-Heal Solo:
- Patient engagement increases (Turner and Ovens, 2018)
- Fewer visits are needed overall
- Healing is promoted (Turner and Ovens, 2017; Guest et al, 2018)
- Patient quality of life is improved (Guest et al, 2018; Turner and Ovens 2018)
- Reliance on pharmacological analgesics, including controlled analgesics, is reduced. This reduction helps prevent escalation up the pain ladder, keeping patients off opioids.
See Table 1 for additional features and related benefits of Accel-Heal Solo.
It is time to more actively embrace new technologies that can stimulate healing in hard-to-heal wounds whilst also reducing wound pain. Accel-Heal Solo is one such evidence-based technology that should now be on every wound clinician’s radar.