After taking on the coordinator role for the 20-credit SQA Level 9 Tissue Viability & Wound Care Module several years ago, I became increasingly concerned over the instructional design, or pedagogy, since no national recommended approach existed. This was particularly important as there had been a noticeable change in the student profile: from acute and primary care nurses to a more international and multidisciplinary healthcare representation, including physiotherapists, care home managers, healthcare assistants and paramedics. There was a noticeable increase in representation from those with backgrounds in mental healthcare, prisons, self-harm and homelessness. Students’ specialist needs were becoming more diverse. The existing ‘one size fits all’ curriculum design was not fitting all — my module content was ‘bursting at the seams’.
To address this, I studied for a Doctorate of Education (EdD) at the University of Strathclyde between 2015–2020 to help understand the most suitable pedagogy, then implement the findings. I wanted to create a student-led pedagogy generated from their everyday, up-close-and-personal and professional experiences.
My main driver was that the module
content – derived from European Wound Management Association EQF Level 7, Wound Management Curriculum for Post Registration Qualification of nurses — was at capacity
[Table 1]. So, I constructed a multi-method sequential qualitative research design comprising three phases:
- critical discourse analysis (CDA)
- directed content analysis (DCA)
- deliberative debate (DD).
The CDA of a corpus from national wound care professional bodies, including the Royal College of Nursing and the Nursing and Midwifery Council, generated two ‘constructs’: Ambiguity or Opportunity? and Responsibility without Accountability, and several ‘subconstructs’ [Table 2]. Using these, I conducted a DCA of content from a sample of anonymised online student discussion posts on the virtual learning platform [Figure 1], identifying four themes:
Theme 1: It’s all a bit ‘hitty-missy’
“I work in [X] health board and as student [A] said, we don’t use honey. The previous board
I worked in, we did.”
“We don’t use honey in [Y] health board and haven’t for many years, [but] when I worked in another practice a few years ago, it was used.”
“I used honey as a case study when I did my dissertation on the specific types of honey used on wounds, mainly leg ulcers, and most of the studies I found supported the use of honey and found good results, especially in wounds colonised with MRSA and pseudomonas.”
“The study included has suggested that there is no conclusive evidence that honey assists the healing of leg ulcers!”
Theme 2: It’s all a question of judgement
“The nurses’ individual judgement definitely accounts for a lot. It would be interesting to analyse the differences between two nurses assessing the same wound to help identify differences in use of the wound chart and differences in individual wound assessment. I have used a decision-making tool to do this before for the Waterlow Scale, using Brunswick’s lens model. Long story short, you need to consider expertise and personal judgement and decision-making and the tool is only the prompt for areas of consideration.”
Theme 3: Too many coaches, not enough players
“The organisation is undergoing a transition from one company to another and some toxic organisational cultures are becoming evident. To be honest, blame culture was always evident…”
“Hospital doctors should be able to prescribe it rather than have nurses rummaging in the
cupboard for dressings. I have seen incontinence pads put on heavy exudating leg ulcers!”
“Silver dressings are scorned and we have to fill in a special rationale form if we want to use it.”
“I think the culture in the hospital is not really focused on holistic care and there are so many other pressures with regard to delayed discharges and other targets that the time to care has gone out the window.”
“I don’t know what we can do to change this as the coaches make the decisions and ultimately, we are just the players.”
Theme 4: Know your rights
“Patients are very informed now; they know their rights. Compliance is a big issue in my area also. I provide equipment such as pressure-relieving cushions or mattresses, then go back and find patients sitting on rubber rings.”
“Now, the problems arose because he was completely unwilling to consent for any investigations of any type. We never even at any time managed to assess the wound fully. He was aggressive and one of my staff ended up with a black eye due to him punching her. He had fallen on the floor and was unable to stand up. We had no other choice but to use the hoist, which was painful for him.”
DCA findings
- The nature of wound care is fundamentally unpredictable and unique
- Conflicting organisational, professional, clinical and individual patient needs take a professional and personal toll
- There are deep-seated and widespread feelings of inequality, inconsistency, contradiction and unpredictability in wound care knowledge, practice, resources and education
- The inherent tension between strong professional ambitions and the drive to heal wounds, and the unstable conditions encountered in practice, often takes its toll on the personal and professional lives of those delivering wound care
- Wound care is multidisciplinary — one size of education does not fit all
- Education should provide practitioners with a skills ‘toolbox’ to enable problem-solving, approaches to conflict resolution, negotiation and ethical dilemmas routinely encountered in practice
- We should move away from content-driven prescriptive standardisation of wound care education to a pedagogy of developing problem-solving processes and techniques
- The unstable conditions in wound care provision have a remarkable similarity to the ‘built, bridged, extended’ (BBE) problem-solving research by Woods et al (1997) — in the entirely unrelated discipline of chemical engineering
- Woods et al noticed most mistakes happen when trying to define the problem: the most successful practitioners draw from a range of metacognitive and cognitive skills [Table 3]
- Woods et al noticed that despite students engaging in problem-solving and using explicit suggestions to solve problems — including sample solutions, open-ended problems and group projects — students still experienced unexpected difficulties
- Just providing students with chances to solve interesting problems was not effective in developing problem-solving skills
- When the wording or context changed the students could not solve the problems — instead they patched various parts of previous situations together to match the new problem situations.
Recommendations
The findings of the DCA indicate general problem-solving skills should be ‘built’ (using content independent activities), ‘bridged’ (to apply skills in a content-specific domain), then ‘extended’ (to use the skills in other contexts and contents and in everyday life).
Further, activities in the wound care curriculum should include developing focus, information gathering, remembering, organisation, analysis, integration, evaluation, flexibility, interpretation and description.
Wound care learning and teaching should be orientated towards wound care professionals acquiring a selected set of cognitive and attitudinal skills that equips them to solve problems by helping them to systematically work with whatever resources and knowledge are available at the time.
It is anticipated BBE will help the problem solvers to overcome the initial distress naturally encountered when beginning an ambiguous and challenging problem, give them a common language to improve communications, and help teams stay on task while improving their confidence and skills in problem-solving.
Where to next in the journey?
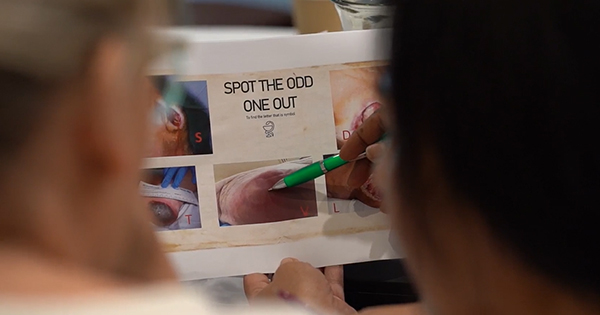
Through the new tripartite curriculum delivery design (which incorporates not only academic but clinical and industry expertise), explicit, content-independent problem-solving exercises have been introduced, intended to develop students’ cognitive and metacognitive skills. This gives students an opportunity to see how to do a skill in a content-independent domain, allowing them to compare their behaviour with the target behaviour. Activities are being introduced to help them develop their behaviour through practice and immediate feedback from peers and module instructors. Tests and assessment of process skills that assess the degree to which students can apply skills are being explored.
Crucially, problem-solving workshops, the processes used to obtain the best answer to an unknown, or decisions subject to some constraints, should enable students to recognise that, for real-world problems, the perfect information is never available, and the best possible answer must therefore be obtained with available resources – an answer that is the ‘best answer’ and subject to some constraints.